| Program Name: | BadgerCare Plus and Medicaid | Handbook Area: | Physician | | 05/17/2024 | Reimbursement : AmountsTopic #258 Acceptance of Payment
The amounts allowed as payment for covered services must be accepted as payment in full. Therefore, total payment for the service (i.e., any amount paid by other health insurance sources, any BadgerCare Plus or Medicaid copayment or spenddown amounts paid by the member, and any amount paid by BadgerCare Plus, Medicaid, or ADAP) may not exceed the allowed amount. As a result, providers may not collect payment from a member, or authorized person acting on behalf of the member, for the difference between their usual and customary charge and the allowed amount for a service (i.e., balance billing).
Other health insurance payments may exceed the allowed amount if no additional payment is received from the member or BadgerCare Plus, Medicaid, or ADAP. Topic #8277 Additional Reimbursement for Reporting Body Mass Index
ForwardHealth is collecting BMI data on children enrolled in BadgerCare Plus or Medicaid to gather baseline information for future policy initiatives.
ForwardHealth will reimburse an additional $10.00 to providers and clinics for reporting BMI on professional claims for routine office visits and preventive services for members two to 18 years old on the DOS.
Providers who are eligible to receive the additional reimbursement include the following:
- HealthCheck agencies
- Nurse midwives
- Nurse practitioners
- Physician assistants
- Physicians
Reporting Body Mass Index on Claims
For the additional reimbursement, CPT Category II procedure code 3008F (Body mass index, documented) is required on the claim in addition to an office visit procedure code. An ICD diagnosis reporting the pediatric BMI outcome must be associated with code 3008F. A $10.00 minimum is required to be billed for procedure code 3008F.
Providers are required to maintain records that fully document the basis of charges upon which all claims for additional reimbursement payments are made.
Reimbursement
Providers are paid $10.00 per billing provider, per child, per calendar year for reporting BMI for members in fee-for-service. Payments for reporting BMI will appear on the RA under EOB code 9944, "Pricing Adjustment - Incentive Pricing." Topic #647 Ancillary Providers
Wisconsin Medicaid covers counseling services (e.g., weight management, diabetic, smoking cessation, and prenatal services), coordination of care services, and delegated medical acts (e.g., giving injections or immunizations, checking medications, changing dressings) provided by ancillary providers if all of the following are true:
- The services are provided under the direct, immediate, on-site supervision of a physician.
- The services are pursuant to the physician's plan of care.
- The supervising physician has not also provided Medicaid reimbursable services during the same office or outpatient E&M visit.
Examples of ancillary providers include non-Medicaid enrollable health care professionals such as staff nurses, dietician counselors, nutritionists, health educators, genetic counselors, and some nurse practitioners. (Nurse practitioners, nurse midwives, and anesthetists who are Medicaid enrolled should refer to their service-specific area for billing information.)
"On-site" means that the supervising physician is in the same building in which services are being provided and is immediately available for consultation or, in the case of emergencies, for direct intervention. The physician is not required to be in the same room as the ancillary provider, unless dictated by medical necessity and good medical practice.
Since ancillary providers are not Medicaid-eligible providers, claims for these services must be submitted under the supervising physician's NPI using the lowest appropriate level office or outpatient visit procedure code or other appropriate CPT code for the service performed. These services are not to be billed in addition to or combined with the physician service if the physician sees the patient during the same visit. Topic #694 Billing Service and Clearinghouse Contracts
According to Wis. Admin. Code § DHS 106.03(5)(c)2, contracts with outside billing services or clearinghouses may not be based on commission in which compensation for the service is dependent on reimbursement from BadgerCare Plus. This means compensation must be unrelated, directly or indirectly, to the amount of reimbursement or the number of claims and is not dependent upon the actual collection of payment. Topic #8117 Electronic Funds Transfer
EFT allows ForwardHealth to directly deposit payments into a provider's designated bank account for a more efficient delivery of payments than the current process of mailing paper checks. EFT is secure, eliminates paper, and reduces the uncertainty of possible delays in mail delivery.
Only in-state and border-status providers who submit claims and MCOs are eligible to receive EFT payments.
Provider Exceptions
EFT payments are not available to the following providers:
- In-state emergency providers
- Out-of-state providers
- Out-of-country providers
- SMV providers during their provisional enrollment period
Enrolling in Electronic Funds Transfer
A ForwardHealth Portal account is required to enroll into EFT as all enrollments must be completed via a secure Provider Portal account or a secure MCO Portal account. Paper enrollments are not accepted. A separate EFT enrollment is required for each financial payer a provider bills.
Providers who do not have a Portal account may Request Portal Access online. Providers may also call the Portal Helpdesk for assistance in requesting a Portal account.
The following guidelines apply to EFT enrollment:
- Only a Portal Administrator or a clerk that has been assigned the "EFT" role on the Portal may complete the EFT enrollment information.
- Organizations can revert back to receiving paper checks by disenrolling in EFT.
- Organizations may change their EFT information at any time.
- Organizations will continue to receive their Remittance Advice as they do currently.
Refer to the Electronic Funds Transfer User Guide on the User Guides page of the Portal for instructions and more information about EFT enrollment.
Providers will continue to receive payment via paper check until the enrollment process moves into "Active" status and the provider's ForwardHealth EFT enrollment is considered complete.
Recoupment and Reversals
Enrollment in EFT does not change the current process of recouping funds. Overpayments and recoupment of funds will continue to be conducted through the reduction of payments.
Note: Enrolling in EFT does not authorize ForwardHealth to make unauthorized debits to the provider's EFT account; however, in some instances an EFT reversal of payment may be necessary. For example, if the system generates a payment twice or the amount entered manually consists of an incorrect value (e.g., a decimal point is omitted creating a $50,000 keyed value for a $500 claim), a reversal will take place to correct the error and resend the correct transaction value. ForwardHealth will notify the designated EFT contact person of an EFT reversal if a payment is made in error due to a system processing or manual data entry error.
Problem Resolution
If payment is not deposited into the designated EFT account according to the ForwardHealth payment cycle, providers should first check with their financial institution to confirm the payment was received. If the payment was not received, providers should then call Provider Services to resolve the issue and payment by paper check will be reinstated until the matter has been resolved. Topic #897 Fee Schedules
Maximum allowable fee information is available on the Max Fee Schedules page of the ForwardHealth Portal in the following forms:
- An interactive maximum allowable fee schedule
- Downloadable fee schedules by service area only in TXT or CSV files
Policy information is not displayed in the fee schedules. Providers should refer to their specific service area in the Online Handbook for more information about coverage policy related to a specific procedure code.
Certain fee schedules are interactive. On the interactive fee schedule, providers have more search options for looking up some coverage information, as well as the maximum allowable fees, as appropriate, for reimbursable HCPCS, CPT, or CDT procedure codes for most services.
Providers have the ability to independently search by:
- A single HCPCS, CPT, or CDT procedure code
- Multiple HCPCS, CPT, or CDT procedure codes
- A pre-populated code range
- A service area (Service areas listed in the interactive fee schedule more closely align with the provider service areas listed in the Online Handbook, including the WCDP programs and WWWP.)
The downloadable fee schedules, which are updated monthly, provide basic maximum allowable fee information by provider service area.
Through the interactive fee schedule, providers can export their search results for a single code, multiple codes, a code range, or by service area. The export function of the interactive fee schedule will return a zip file that includes seven CSV files containing the results.
Note: The interactive fee schedule will export all associated information related to the provider's search criteria except the procedure code descriptions.
Providers may call Provider Services in the following cases:
- The ForwardHealth Portal is not available.
- There is uncertainty as to which fee schedule should be used.
- The appropriate fee schedule cannot be found on the Portal.
- To determine coverage or maximum allowable fee of procedure codes not appearing on a fee schedule.
Topic #19777 Targeted Reimbursement Rate Increase
In accordance with a provision of the 2015-17 biennial state budget (2015 Wisconsin Act 55), ForwardHealth implemented a targeted enhanced reimbursement rate for pediatric dental care and certain adult dental services. The targeted reimbursement rate applies to all Medicaid-enrolled provider types eligible to render dental services and applies to services rendered in Brown, Marathon, Polk, and Racine counties. The rendering provider's practice location is considered the county where the services are rendered, not the county of the billing provider or the member.
The reimbursement rate increase applies to all Medicaid-enrolled provider types eligible to render dental services in a target county; however, the reimbursement rate increase does not apply to dental services billed through a federally qualified health center. The reimbursement rate applies to services provided fee-for-service and via managed care.
If the rendering provider practices in both a target county and non-target county, the rendering provider is required to obtain separate Medicaid enrollment for both the target county and the non-target county. The address of the rendering provider should be indicated in the appropriate field on submitted claims, including the zip code matching the Medicaid enrollment address. Rendering providers who need to set up separate Medicaid enrollment for separate locations can begin the process as follows:
- Go to the Provider Enrollment page.
- Click the Start or Continue Your Enrollment Application link to begin a new Medicaid enrollment.
Providers with questions regarding the enrollment process can call ForwardHealth Provider Services.
Maximum Allowable Fees
ForwardHealth reimburses the lesser of the provider's billed amount or the increased reimbursement rate. The maximum daily reimbursement rate policy applies only for services eligible for the rate increase.
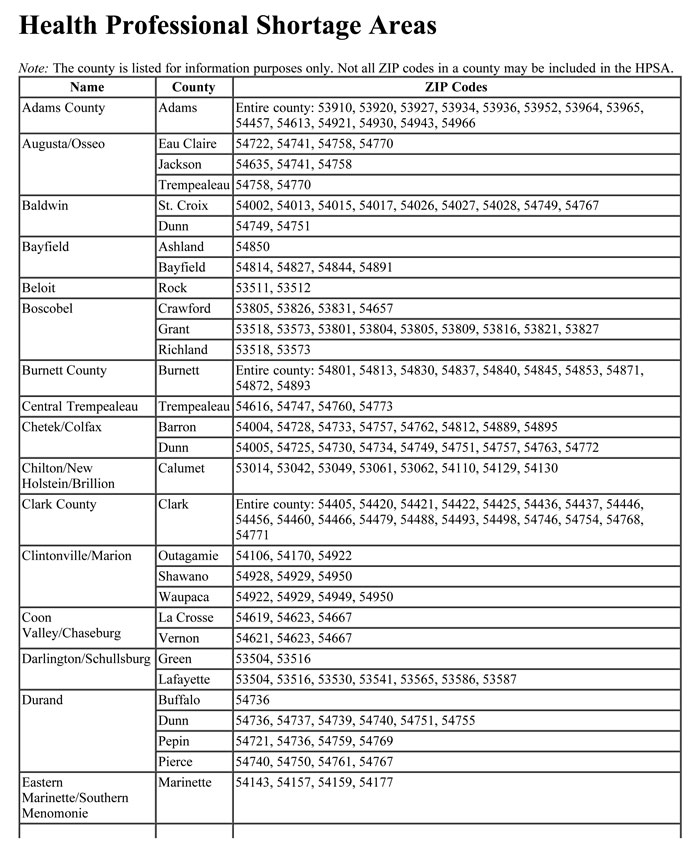
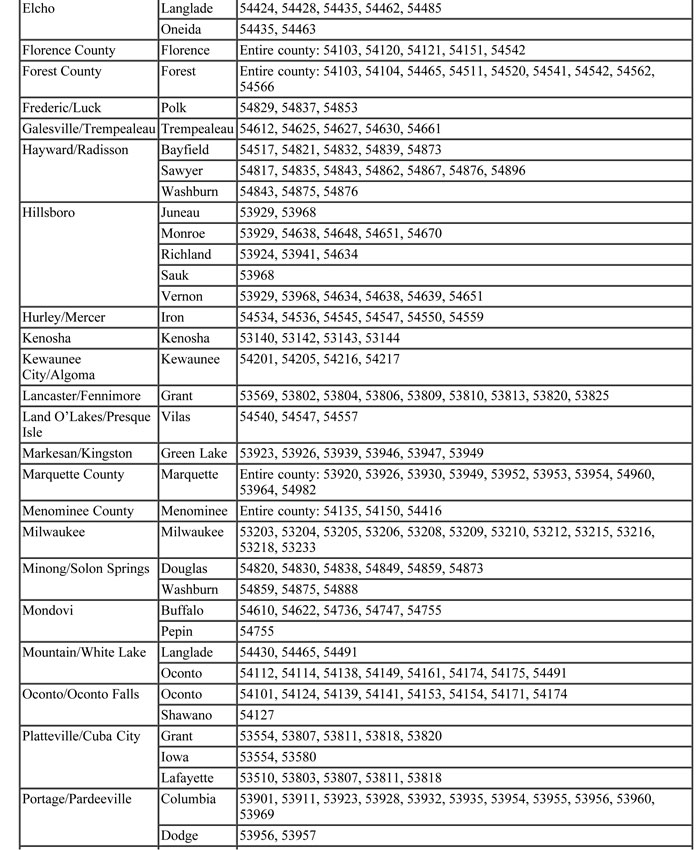
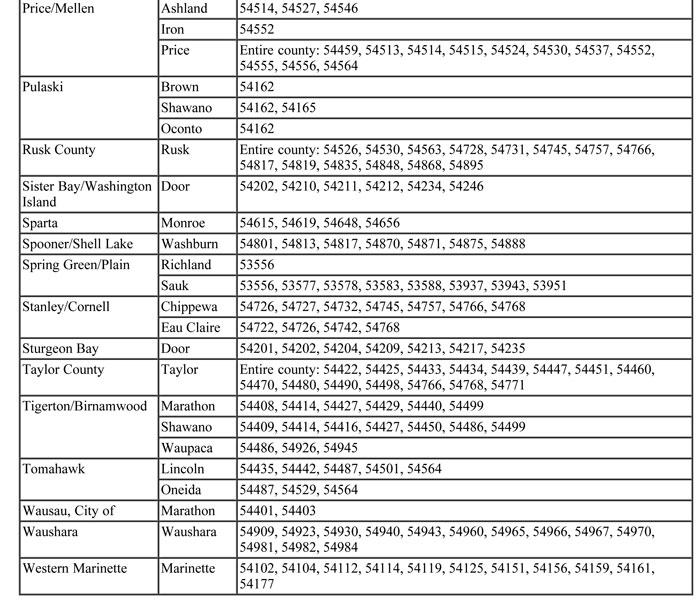
The maximum allowable fee schedule includes all current reimbursement rates. Providers should indicate their usual and customary charges when submitting claims for services. Topic #648 Health Professional Shortage Areas
Enhanced reimbursement is provided to Medicaid-enrolled primary care providers and emergency medicine providers for selected services when one or both of the following apply:
- The rendering or billing provider is located in a HPSA-eligible ZIP code.
- The member has a residential address (according to enrollment records) within a HPSA-eligible ZIP code.
Primary care providers and emergency medicine providers include the following:
- Physicians with specialties of general practice, obstetrics and gynecology, family practice, internal medicine, or pediatrics
- Physician assistants
- Nurse practitioners
- Nurse midwives
Standard enhanced reimbursement for HPSA-eligible primary care procedures is an additional 20 percent of the physician maximum allowable fee. The enhanced reimbursement for HPSA-eligible obstetrical procedures is an additional 50 percent of the physician maximum allowable fee.
Health Professional Shortage Area-Eligible Procedure Codes
Providers may use HPSA modifier AQ (Physician providing a service in a HPSA) with the following categories of procedure codes (while the AQ modifier is defined for physicians only, any Medicaid HPSA-eligible provider may use the modifier when appropriate):
- E&M Office Visits, New Patient
- E&M Office Visits, Established Patient
- E&M Home Visits, New Patient
- E&M Home Visits, Established Patient
- Emergency Department Services
- Newborn Care
- Preventive Medicine
- Obstetric Care
- Vaccines
Use of Modifier AQ
To obtain the HPSA-enhanced reimbursement, providers are required to indicate modifier AQ along with the appropriate procedure code on the claim. (Refer to the Pediatric Services Performed in a Health Professional Shortage Area section of this topic for information regarding use of modifier AQ for pediatric services.)
Medicare Crossover Claims
Medicare HPSA policy differs from Wisconsin Medicaid's HPSA policy in many ways. Medicaid covers more services than Medicare, allows a broader range of providers to receive the incentive payment, pays a higher bonus, and defines HPSA differently than Medicare. Most importantly, Wisconsin Medicaid pays the enhanced reimbursement to physicians, physician assistants, nurse practitioners, and nurse midwives while Medicare pays the HPSA incentive payment only to physicians.
For these reasons, Medicare crossover claims that are eligible for the Medicaid HPSA incentive payment may not automatically be forwarded to ForwardHealth from Medicare. Providers may have to submit these claims directly to ForwardHealth.
Antepartum Care Visits Performed in a Health Professional Shortage Area
If a provider renders three or fewer antepartum care visits, the provider is required to bill the appropriate E&M service code with modifier TH (Obstetrical treatment/services, prenatal or postpartum) listed first and the HPSA modifier AQ listed second.
If a provider renders three or fewer antepartum care visits and the rendering provider is a licensed midwife, the provider is required to bill procedure code 59425 with modifier 52 (representing antepartum care only; less than 4 visits) listed first and the HPSA modifier AQ listed second.
Pediatric Services Performed in a Health Professional Shortage Area
Pediatric services include office and other outpatient services and emergency department services for members 18 years of age and younger.
Reimbursement for eligible procedure codes with HPSA modifier AQ automatically includes the pediatric incentive payment, when applicable, since the incentive payment is based on the age of the member. Providers should not submit claims with modifier TJ in addition to HPSA modifier AQ for the same procedure code. Providers should only include the HPSA modifier in situations where both of these modifiers apply. Wisconsin Medicaid will determine the member's age and determine the proper HPSA reimbursement for these procedure codes.
Modifier TJ may be used when submitting claims for eligible services in situations that do not qualify for HPSA-enhanced reimbursement.
HealthCheck Services Not Eligible for Health Professional Shortage Area Incentive Payment
Procedure codes 99381-99385 and 99391-99395 are not eligible for HPSA incentive payments, regardless of the billing or rendering provider's or member's location, since reimbursement for these procedure codes includes enhanced reimbursement for HealthCheck services.
Claims Submitted Inappropriately for Health Professional Shortage Area Incentive Payment
Providers who submit claims for the HPSA-enhanced reimbursement inappropriately are reimbursed the lesser of the provider's usual and customary fee or the maximum allowable fee, assuming that all other ForwardHealth policies are followed. The enhanced reimbursement amount is not paid when the HPSA modifier is submitted but the provider or member is not eligible for HPSA designation.
 Topic #3510 HealthCheck Services
Wisconsin Medicaid provides enhanced reimbursement for comprehensive health screens for members under age 21 when those screens are billed as HealthCheck services (CPT procedure codes 99381-99385 and 99391-99395). Topic #260 Maximum Allowable Fees
Maximum allowable fees are established for most covered services. Maximum allowable fees are based on various factors, including a review of usual and customary charges submitted, the Wisconsin State Legislature's Medicaid budgetary constraints, and other relevant economic limitations. Maximum allowable fees may be adjusted to reflect reimbursement limits or limits on the availability of federal funding as specified in federal law.
Providers are reimbursed at the lesser of their billed amount and the maximum allowable fee for the procedure. Topic #649 Maximum Daily Reimbursement
ForwardHealth reimbursement for services performed on the same DOS for the same member by the same rendering provider is limited to $2,331.37 for services rendered by the following providers:
- Anesthesiologists
- Anesthesiologist Assistants
- Certified Registered Nurse Anesthetists
- Licensed midwives
- Nurse Midwives
- Nurse Practitioners
- Physician Assistants
- Physicians
- Podiatrists
The maximum daily reimbursement amount does not apply to physician-administered drugs and DME.
Dental services, including radiographs (when submitted on a dental claim) and oral surgery emergency services, are subject to a different maximum daily reimbursment amount.
ForwardHealth remittance information will indicate when the maximum daily reimbursement amount has been met.
Requests to Exceed Maximum Daily Reimbursement Limit
Providers may request additional reimbursement to exceed the maximum daily reimbursement limit when both of the following criteria are met:
- A surgery exceeds 6 hours or anesthesia exceeds 7.5 hours.
- The Medicaid-allowed amount for the services meets or exceeds the maximum daily reimbursement limit.
Submitting Supporting Documentation
To request reimbursement in excess of the maximum daily reimbursement limit, providers are required to submit the following information on the claim:
- In the Notes field, indicate "request for additional reimbursement for surgery in excess of 6 hours," or "request for additional reimbursement for anesthesia services in excess of 7.5 hours."
- Attach supporting documentation to the claim that clearly indicates the length of the surgery or the length of the anesthesia services, such as a post-operative report.
Providers are reminded of the following options for providing supporting documentation along with a claim:
- On paper with supporting documentation submitted on paper.
- Electronically using DDE through the Portal, PES transactions, or 837 Health Care Claim electronic transactions. For more information, refer to the User Guides page of the ForwardHealth Portal.
- Electronically with an indication that supporting documentation will be submitted separately on paper. For more information, refer to the ForwardHealth Companion Guides.
Topic #866 Nurse Practitioners
Nurse practitioners are reimbursed the lesser of the nurse practitioner's usual and customary charge for a service or the physician's maximum allowable fee for the procedure. Nurse practitioners use the physician maximum allowable fee schedule. Topic #650 Pediatric Services
Wisconsin Medicaid provides an enhanced reimbursement rate for office and other outpatient services (CPT procedure codes 99202–99215 and HCPCS procedure code G2212) and emergency department services (CPT procedure codes 99281–99285) for members 18 years of age and younger. The enhanced reimbursement rates are indicated on the physician services maximum allowable fee schedule.
To obtain the enhanced reimbursement for members under 18 years old, indicate the applicable procedure code and modifier "TJ" (Program group, child and/or adolescent) on the claim. Topic #651 Physician Assistants
Wisconsin Medicaid generally reimburses physician assistants 90 percent of the payment allowed for the physician who would have otherwise performed the service. Physician assistants are paid 100 percent of the physician's maximum fee for HealthCheck screens, injections, immunizations, lab handling fees, and select diagnostic procedures. Topic #652 Physicians
Wisconsin Medicaid reimburses physicians the lesser of the physician's billed amount for a service or Wisconsin Medicaid's maximum allowable fee. Topic #553 Psychiatric and Substance Abuse Services
To be reimbursed for psychiatric services (CPT codes 90785-90853, 90865-90899), physicians are required to be certified as a psychiatrist pursuant to Wis. Admin. Code DHS 105.22(1)(a).
Any Medicaid-enrolled physician may be reimbursed for substance abuse services. Topic #7777 Reimbursement Rates for Professional Services
For most professional services, ForwardHealth reimburses no more than Medicare rates. However, for select professional services, the rate for the service is greater than the Medicare rate when provided to members 18 years of age and younger on the date of service.
Providers should refer to the Medicaid maximum allowable fee schedule on the ForwardHealth Portal for current reimbursement rates.Topic #13297 Reimbursement for Office-Based Services Provided in a Hospital or an Ambulatory Surgery Center
ForwardHealth reduces reimbursement to physicians and other professional service providers for services that are typically provided in an office-based setting when those services are instead provided in a hospital (POS code 21 or 22) or an ASC (POS code 24). The reduced reimbursement is intended to account for the lower overhead costs typically realized by physicians and other professional services providers when services are provided in a hospital or an ASC.
Refer to the table below for the affected codes. The reduced reimbursement for these services when provided in a hospital or an ASC equals 80 percent of maximum allowable fees.
Affected services are reimbursed at the full maximum allowable fee when provided in an allowable POS other than 21, 22, or 24.
For select services (identified on the table by an asterisk), reimbursement reductions apply only for members who are 19 years of age or older on the DOS. For these select services, providers are reimbursed at the full maximum allowable fee when the service is rendered to members who are 18 years of age or younger on the DOS, regardless of POS.
| 10005 |
10007 |
10009 |
10021 |
10030 |
10040 |
10060 |
10061 |
10080 |
10081 |
| 10120 |
10121 |
10140 |
10160 |
11000 |
11001 |
11042 |
11055 |
11056 |
11057 |
| 11200 |
11201 |
11300 |
11301 |
11302 |
11303 |
11305 |
11306 |
11307 |
11308 |
| 11310 |
11311 |
11312 |
11313 |
11400 |
11401 |
11402 |
11403 |
11404 |
11406 |
| 11420 |
11421 |
11422 |
11423 |
11424 |
11426 |
11440 |
11441 |
11442 |
11443 |
| 11444 |
11446 |
11600 |
11601 |
11602 |
11603 |
11604 |
11606 |
11620 |
11621 |
| 11622 |
11623 |
11624 |
11626 |
11640 |
11641 |
11642 |
11643 |
11644 |
11646 |
| 11719 |
11720 |
11721 |
11730 |
11732 |
11740 |
11750 |
11755 |
11765 |
11900 |
| 11901 |
11950 |
11951 |
11952 |
11954 |
11971 |
11976 |
11980 |
11981 |
11982 |
| 11983 |
12020 |
12021 |
15851 |
16000 |
16020 |
16025 |
16030 |
17000 |
17003 |
| 17004 |
17106 |
17107 |
17108 |
17110 |
17111 |
17250 |
17260 |
17261 |
17262 |
| 17263 |
17264 |
17266 |
17270 |
17271 |
17272 |
17273 |
17274 |
17276 |
17280 |
| 17281 |
17282 |
17283 |
17284 |
17286 |
17311 |
17312 |
17313 |
17314 |
17315 |
| 17340 |
17360 |
19000 |
19001 |
19030 |
19100 |
19101 |
20526 |
20550 |
20551 |
| 20552 |
20553 |
20600 |
20604 |
20605 |
20606 |
20610 |
20611 |
20612 |
20615 |
| 21073 |
21076 |
21077 |
21079 |
21080 |
21081 |
21082 |
21083 |
21084 |
21085 |
| 21086 |
21087 |
21088 |
23350 |
23500 |
23505 |
23520 |
23525 |
23540 |
23545 |
| 23570 |
23575 |
23620 |
23625 |
24500 |
24505 |
24530 |
24535 |
24560 |
24565 |
| 24576 |
24577 |
24640 |
24650 |
24655 |
24670 |
24675 |
25246 |
25500 |
25505 |
| 25520 |
25530 |
25535 |
25560 |
25565 |
25600 |
25605 |
25622 |
25624 |
25630 |
| 25635 |
25650 |
25675 |
26010 |
26011 |
26600 |
26605 |
26641 |
26645 |
26670 |
| 26675 |
26700 |
26705 |
26720 |
26725 |
26740 |
26742 |
26750 |
26755 |
26770 |
| 26775 |
27093 |
27095 |
27096 |
27220 |
27230 |
27246 |
27256 |
27500 |
27501 |
| 27508 |
27516 |
27520 |
27530 |
27532 |
27538 |
27550 |
27560 |
27648 |
27656 |
| 27750 |
27752 |
27760 |
27762 |
27767 |
27780 |
27781 |
27786 |
27788 |
27808 |
| 27810 |
27816 |
27818 |
27824 |
27825 |
27830 |
28400 |
28405 |
28430 |
28435 |
| 28450 |
28455 |
28470 |
28475 |
28490 |
28495 |
28510 |
28515 |
28530 |
28540 |
| 28545 |
28570 |
28575 |
28600 |
28605 |
28630 |
28635 |
28660 |
28665 |
29000 |
| 29010 |
29015 |
29035 |
29040 |
29044 |
29046 |
29049 |
29055 |
29058 |
29065 |
| 29075 |
29085 |
29086 |
29105 |
29125 |
29126 |
29130 |
29131 |
29200 |
29240 |
| 29260 |
29280 |
29305 |
29325 |
29345 |
29355 |
29358 |
29365 |
29405 |
29425 |
| 29435 |
29440 |
29445 |
29450 |
29505 |
29515 |
29520 |
29530 |
29540 |
29550 |
| 29580 |
29581 |
29700 |
29705 |
29710 |
29720 |
29730 |
29740 |
29750 |
30300 |
| 30801 |
30802 |
30901 |
30903 |
30905 |
30906 |
31000 |
31002 |
31231 |
31233 |
| 31235 |
31237 |
31238 |
31295 |
31296 |
31297 |
31505 |
31510 |
31511 |
31512 |
| 31515 |
31525 |
31570 |
31575 |
31576 |
31577 |
31578 |
31579 |
31615 |
36000 |
| 36400 |
36405 |
36406 |
36410 |
36416 |
36470 |
36471 |
36473 |
36475 |
36476 |
| 36478 |
36479 |
36600 |
36901 |
37765 |
37766 |
38220 |
38221 |
40490 |
40500 |
| 40510 |
40520 |
40530 |
40650 |
40652 |
40654 |
40800 |
40801 |
40804 |
40805 |
| 40806 |
40808 |
40810 |
40812 |
40814 |
40816 |
40818 |
40819 |
40820 |
40830 |
| 40831 |
40840 |
40842 |
40843 |
40844 |
40845 |
41000 |
41005 |
41006 |
41007 |
| 41008 |
41009 |
41010 |
41015 |
41016 |
41017 |
41018 |
41100 |
41105 |
41108 |
| 41110 |
41112 |
41113 |
41115 |
41116 |
42100 |
42400 |
42405 |
42650 |
42660 |
| 42700 |
42720 |
42725 |
42800 |
42804 |
42806 |
42808 |
42809 |
45300 |
45303 |
| 45305 |
45307 |
45308 |
45309 |
45315 |
45317 |
45320 |
45321 |
45327 |
46083 |
| 46220 |
46221 |
46320 |
46600 |
46604 |
46606 |
46608 |
46610 |
46611 |
46612 |
| 46614 |
46615 |
46900 |
46910 |
46916 |
46917 |
46922 |
46924 |
46930 |
46940 |
| 46942 |
46945 |
46946 |
51100 |
51101 |
51102 |
51600 |
51610 |
51700 |
51701 |
| 51702 |
51703 |
51705 |
51710 |
51715 |
51720 |
51725 |
51726 |
51727 |
51728 |
| 51729 |
51736 |
51741 |
51784 |
51785 |
51792 |
51797 |
51798 |
52000 |
52001 |
| 52005 |
52007 |
52010 |
52204 |
52214 |
52224 |
52265 |
52270 |
52275 |
52281 |
| 52283 |
52285 |
52310 |
52315 |
53600 |
53601 |
53620 |
53621 |
53660 |
53661 |
| 53850 |
53852 |
53855 |
53860 |
54000 |
54001 |
54050 |
54055 |
54056 |
54057 |
| 54060 |
54065 |
54100 |
54105 |
54200 |
54450 |
55200 |
55250 |
55700 |
56405 |
| 56420 |
56440 |
56441 |
56501 |
56515 |
56605 |
56606 |
56820 |
56821 |
57061 |
| 57065 |
57100 |
57105 |
57160 |
57170 |
57180 |
57420 |
57421 |
57452 |
57454 |
| 57455 |
57456 |
57460 |
57461 |
57500 |
57505 |
57510 |
57511 |
57513 |
57520 |
| 57522 |
57800 |
58100 |
58110 |
58300 |
58301 |
58340 |
58353 |
58356 |
58555 |
| 58558 |
58562 |
58563 |
58565 |
59000 |
59015 |
59020 |
59025 |
59425 |
59426 |
| 59430 |
60000 |
60100 |
60300 |
62280 |
62281 |
62282 |
62284 |
62290 |
62291 |
| 62292 |
62294 |
62367 |
62368 |
64405 |
64408 |
64417 |
64418 |
64420 |
64421 |
| 64430 |
64435 |
64445 |
64450 |
64455 |
64479 |
64480 |
64483 |
64484 |
64490 |
| 64491 |
64492 |
64493 |
64494 |
64495 |
64505 |
64530 |
64553 |
64555 |
64561 |
| 64566 |
64600 |
64605 |
64610 |
64611 |
64612 |
64616 |
64617 |
64620 |
64630 |
| 64632 |
64640 |
64642 |
64643 |
64644 |
64645 |
64646 |
64647 |
64650 |
64653 |
| 64680 |
64681 |
65205 |
65210 |
65220 |
65222 |
65270 |
65272 |
65275 |
65286 |
| 65400 |
65410 |
65420 |
65426 |
65430 |
65435 |
65436 |
65450 |
65600 |
65772 |
| 65778 |
65779 |
65800 |
65815 |
65855 |
65860 |
66020 |
66030 |
66130 |
66183 |
| 66250 |
66700 |
66710 |
66720 |
66740 |
66761 |
66762 |
66770 |
66821 |
67025 |
| 67028 |
67101 |
67105 |
67110 |
67120 |
67141 |
67145 |
67208 |
67210 |
67220 |
| 67221 |
67225 |
67227 |
67228 |
67500 |
67505 |
67515 |
67700 |
67710 |
67715 |
| 67800 |
67801 |
67805 |
67810 |
67820 |
67825 |
67830 |
67840 |
67850 |
67875 |
| 67880 |
67882 |
67900 |
67901 |
67903 |
67904 |
67908 |
67909 |
67912 |
67914 |
| 67915 |
67916 |
67917 |
67921 |
67922 |
67923 |
67924 |
67930 |
67935 |
67938 |
| 67950 |
67961 |
67966 |
68020 |
68040 |
68100 |
68110 |
68115 |
68130 |
68135 |
| 68200 |
68320 |
68330 |
68340 |
68360 |
68400 |
68420 |
68440 |
68510 |
68530 |
| 68705 |
68760 |
68761 |
68801 |
68810 |
68815 |
68816 |
68840 |
68850 |
69000 |
| 69005 |
69020 |
69100 |
69105 |
69110 |
69145 |
69200 |
69210 |
69220 |
69222 |
| 69300 |
69420 |
69433 |
69540 |
90912 |
90913 |
92612 |
92613 |
92614 |
92615 |
| 92616 |
92617 |
92640 |
93000 |
93005 |
93015 |
93017 |
93040 |
93041 |
93224 |
| 93225 |
93226 |
93227 |
93228 |
93229 |
93268 |
93270 |
93271 |
93272 |
93278 |
| 93279 |
93280 |
93281 |
93282 |
93283 |
93284 |
93285 |
93288 |
93289 |
93290 |
| 93291 |
93292 |
93293 |
93294 |
93295 |
93296 |
93297 |
93298 |
93303 |
93304 |
| 93306 |
93307 |
93308 |
93320 |
93321 |
93325 |
93350 |
93351 |
93352 |
93880 |
| 93882 |
93922 |
93923 |
93924 |
93925 |
93926 |
93930 |
93931 |
93970 |
93971 |
| 93975 |
93976 |
93978 |
93979 |
93980 |
93981 |
93990 |
94010 |
94060 |
94070 |
| 94150 |
94200 |
94375 |
94450 |
94452 |
94453 |
94660 |
94680 |
94681 |
94690 |
| 94760 |
95004 |
95012 |
95024 |
95027 |
95028 |
95044 |
95052 |
95056 |
95060 |
| 95065 |
95070 |
95801 |
95805 |
95806 |
95807 |
95808 |
95810 |
95811 |
95812 |
| 95813 |
95816 |
95819 |
95830 |
95851 |
95852 |
95857 |
95860 |
95861 |
95863 |
| 95864 |
95865 |
95866 |
95867 |
95868 |
95869 |
95870 |
95872 |
95873 |
95874 |
| 95875 |
95905 |
95921 |
95922 |
95923 |
95925 |
95926 |
95927 |
95930 |
95933 |
| 95957 |
95970 |
95971 |
95972 |
95980 |
95981 |
95982 |
95990 |
95991 |
95992 |
| 96000 |
96001 |
96002 |
96003 |
96004 |
96105 |
96110 |
96116 |
96125 |
96450 |
| 96542 |
97597 |
97598 |
97605 |
97606 |
97750 |
97760 |
97763 |
98925 |
98926 |
| 98927 |
98928 |
98929 |
99170 |
99173 |
99202* |
99203* |
99204* |
99205* |
99211* |
| 99212* |
99213* |
99214* |
99215* |
99242* |
99243* |
99244* |
99245* |
99381 |
99382 |
| 99383 |
99384 |
99385 |
99386 |
99387 |
99391 |
99392 |
99393 |
99394 |
99395 |
| 99396 |
99397 |
G0101 |
G0102 |
G0104 |
G2212* |
|
|
|
|
* For these select procedure codes, reimbursement reductions apply only for members who are 19 years of age or older on the DOS. Topic #653 Residents
Wisconsin Medicaid reimburses residents for physician services when:
- The resident is fully licensed to practice medicine and has obtained an NPI.
- The service can be separately identified from those services that are required as part of the training program.
- The resident is operating independently and not under the direct supervision of a physician.
- The service is provided in a clinic, an outpatient hospital, or emergency department setting.
The reimbursement for residents is identical to other licensed physicians. Topic #655 Supervising Physicians of Interns and Residents
Wisconsin Medicaid reimburses supervising physicians in a teaching setting for the services provided by interns and residents if those services are supervised, provided as part of the training program, and billed under the supervising physician's NPI. The supervising physician must provide personal and identifiable direction to interns or residents who are participating in the care of the member. This direction includes any or all of the following:
- Reviewing the member's medical history or physical examination
- Personally examining the member within a reasonable period after admission
- Confirming or revising diagnoses
- Determining the course of treatment to be followed
- Making frequent review of the member's progress
The notes must indicate that the supervising physician personally reviewed the member's medical history, performed a physical and/or psychiatric examination, confirmed or revised the diagnosis, and discharged the member. Topic #656 Surgical Procedures
Surgical procedures performed by the same physician, for the same member, on the same DOS must be submitted on the same claim form. Surgeries that are billed on separate claim forms are denied.
Certain surgical procedures billed on professional claims (i.e., the 837P transaction or the 1500 Health Insurance Claim Form) may be reimbursed only when performed in an inpatient hospital or an ASC.
Reimbursement for most surgical procedures includes reimbursement for preoperative and postoperative care days. Preoperative and postoperative surgical care includes the preoperative evaluation or consultation, postsurgical E&M services (i.e., hospital visits, office visits), suture, and cast removal.
Although E&M services pertaining to the surgery for DOS during the preoperative and postoperative care days are not covered, an E&M service may be reimbursed if it was provided in response to a different diagnosis.
Co-Surgeons
ForwardHealth reimburses each surgeon at 100 percent of ForwardHealth's usual surgeon rate for the specific procedure they have performed. Attach supporting clinical documentation (such as an operative report) clearly marked "co-surgeon" to each surgeon's paper claim to demonstrate medical necessity.
Surgical Assistance
ForwardHealth reimburses surgical assistance services at 20 percent of the reimbursement rate allowed for the provider type for the surgical procedure. To receive reimbursement for surgical assistance, indicate the surgery procedure code with the appropriate assistant surgeon modifier ("80," "81," "82," or "AS") on the claim.
ForwardHealth will automatically calculate the appropriate reimbursement for assistant surgeon services based on the provider type performing the procedure.
Bilateral Surgeries
Bilateral surgical procedures are paid at 150 percent of the maximum allowable fee for the single service. Indicate modifier "50" (bilateral procedure) and a quantity of 1.0 on the claim.
Multiple Surgeries
Multiple surgical procedures performed by the same physician for the same member during the same surgical session are reimbursed at 100 percent of the maximum allowable fee for the primary procedure, 50 percent for the secondary procedure, 25 percent for the tertiary procedure, and 13 percent for all subsequent procedures. The Medicaid-allowed surgery with the greatest usual and customary charge on the claim is reimbursed as the primary surgical procedure, the next highest is the secondary surgical procedure, etc.
ForwardHealth permits full maximum allowable payments for surgeries that are performed on the same DOS but at different surgical sessions. For example, if a provider performs a sterilization on the same DOS as a delivery, the provider may be reimbursed the full maximum allowable fee for both procedures if performed at different times (and if all of the billing requirements were met for the sterilization).
To obtain full reimbursement, submit a claim for all the surgeries performed on the same DOS that are being billed for the member. Then submit an Adjustment/Reconsideration Request for the allowed claim with additional supporting documentation clarifying that the surgeries were performed in separate surgical sessions.
Note: Most diagnostic and certain vascular injection and radiological procedures are not subject to the multiple surgery reimbursement limits. Call Provider Services for more information about whether a specific procedure code is subject to these reimbursement limits.
Multiple Births
Reimbursement for multiple births is dependent on the circumstances of the deliveries. If all deliveries are vaginal or if all are Cesarean, the first delivery is reimbursed at 100 percent of ForwardHealth's maximum allowable fee for the service. The second delivery is reimbursed at 50 percent, the third at 25 percent, and subsequent deliveries at 13 percent each.
In the event of a combination of vaginal and Cesarean deliveries, the delivery with the largest billed amount is reimbursed at 100 percent, the delivery with the next largest at 50 percent, and so on, consistent with the policy for other situations of multiple surgeries.
For example, if the initial delivery of triplets is vaginal and the subsequent two deliveries are Cesarean, the first Cesarean delivery is reimbursed at 100 percent, the second Cesarean delivery at 50 percent, and the vaginal delivery at 25 percent.
Preoperative and Postoperative Care
Reimbursement for certain surgical procedures includes the preoperative and postoperative care days associated with that procedure. Preoperative and postoperative surgical care includes the preoperative evaluation or consultation, postsurgical E&M services (i.e., hospital visits, office visits), suture, and cast removal.
Note: Separate reimbursement is allowed for postoperative management when it is performed by a provider other than the surgeon or shared with the surgeon following cataract surgery.
All primary surgeons, surgical assistants, and co-surgeons are subject to the same preoperative and postoperative care limitations for each procedure. For surgical services in which a preoperative period applies, the preoperative period is typically three days. Claims for services that fall within the range of established pre-care and post-care days for the procedure(s) being performed are denied unless they indicate a circumstance or diagnosis code unrelated to the surgical procedure.
For the number of preoperative and postoperative care days applied to a specific procedure code, call Provider Services. |