| Program Name: | BadgerCare Plus and Medicaid | Handbook Area: | Radiology | | 05/10/2024 | Prior Authorization : Follow-Up to DecisionsTopic #10717 Appeals
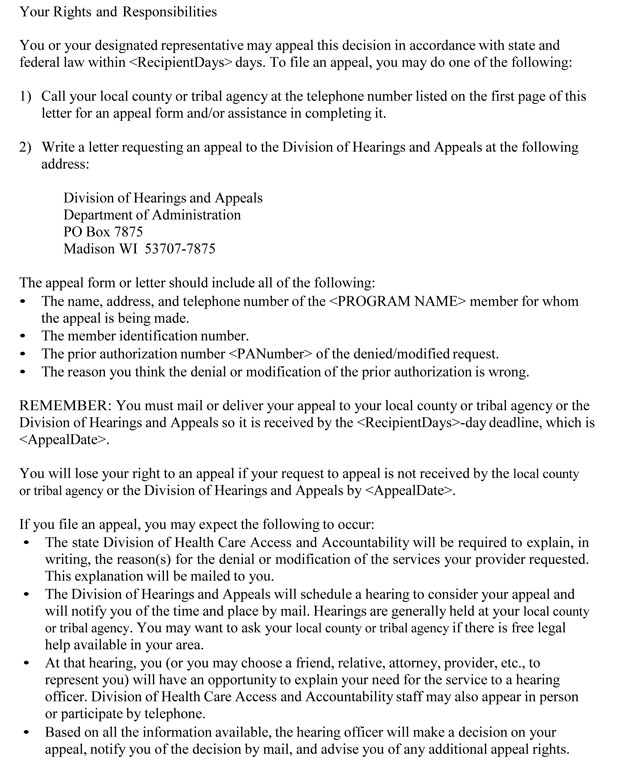
If a PA request is denied or modified by eviCore healthcare, only a member, or authorized person acting on behalf of the member, may file an appeal with the DHA. Decisions that may be appealed include denial or modification of a PA request.
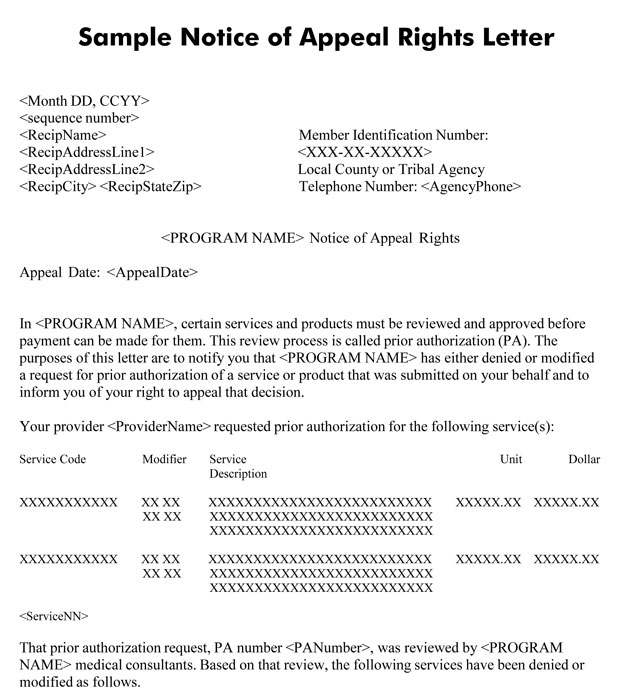
The member is required to file an appeal within 45 days of the date of the Notice of Appeal Rights letter.
To file an appeal, members may complete and submit a Request for Fair Hearing form.
Though providers cannot file an appeal, they are encouraged to remain in contact with the member during the appeal process. Providers may offer the member information necessary to file an appeal and help present their case during a fair hearing.
Fair Hearing Upholds ForwardHealth's Decision
If the hearing decision upholds the decision to deny or modify a PA request, the DHA notifies the member and ForwardHealth in writing. The member may choose to receive the denied service (or in the case of a modified PA request, the originally requested service) as a noncovered service, not receive the service at all, or appeal the decision.
Fair Hearing Overturns ForwardHealth's Decision
If the hearing decision overturns the decision to deny or modify the PA request, the DHA notifies ForwardHealth and the member. The letter includes instructions for the provider and for ForwardHealth.
If the DHA letter instructs the provider to submit a claim for the service, the provider should submit the following to ForwardHealth after the service(s) has been performed:
- A paper claim with "HEARING DECISION ATTACHED" written in red ink at the top of the claim
- A copy of the hearing decision
- A copy of the denied PA request
Providers are required to submit claims with hearing decisions to the following address:
ForwardHealth
Specialized Research
Ste 50
313 Blettner Blvd
Madison WI 53784
Claims with hearing decisions sent to any other address may not be processed appropriately.
If the DHA letter instructs the provider to submit a new PA request, the provider is required to submit the new PA request to eviCore healthcare via fax with a copy of the hearing decision. Providers should clearly indicate that the PA request is for a fair hearing decision and should indicate the requested authorization date. If the service has already been performed, the requested authorization date should be the DOS. If the service has not been performed, the requested authorization date should be the earliest date that the service may be performed. eviCore healthcare does not accept PA requests for overturned hearing decisions via telephone or eviCore healthcare Portal.
eviCore healthcare will then approve the PA request for the overturned hearing decision. When a PA request is approved after an appeal, the provider who submitted the PA request receives a PA confirmation fax. Ordering providers are encouraged to share the information on the PA confirmation fax with the provider who rendered or will render the service. The provider rendering the service may then submit a claim following the usual claims submission procedures after providing the service(s).
Financial Responsibility
If the member asks to receive the service before the hearing decision is made, the provider is required to notify the member before rendering the service that the member will be responsible for payment if the decision to deny or modify the PA request is upheld.
If the member accepts responsibility for payment of the service before the hearing decision is made, and if the appeal decision upholds the decision to deny or modify the PA request, the provider may collect payment from the member if certain conditions are met.
If the member accepts responsibility for payment of the service before the hearing decision is made, and if the appeal decision overturns the decision to deny or modify a PA request, the provider may submit a claim to ForwardHealth. If the provider collects payment from the member for the service before the appeal decision is overturned, the provider is required to refund the member for the entire amount of payment received from the member after the provider receives Medicaid's reimbursement.
Wisconsin Medicaid does not directly reimburse members.
 |