| Program Name: | BadgerCare Plus and Medicaid | Handbook Area: | Radiology | | 05/07/2024 | Prior Authorization : DecisionsTopic #10697 Approved Requests
PA requests for advanced imaging services are approved by eviCore healthcare for a period of 60 calendar days from the grant date. The provider who submitted the PA request receives a copy of a PA confirmation fax when a PA request for a service is approved. Ordering providers are encouraged to share the information on the PA confirmation fax with the provider who renders the service. Providers may render the approved services beginning on the grant date.
The PA confirmation fax identifies the specific procedure codes that are approved. The provider who renders the service may substitute and perform a service defined by a different procedure code without contacting eviCore healthcare only when the substituted procedure code is considered a "downcode," as in the following situations:
- The provider renders a service without contrast when the approved service included contrast or included scans both with and without contrast.
- The provider renders a service with contrast when the approved service included scans both with and without contrast.
For example, if the PA confirmation fax authorizes procedure code 70470 (Computed tomography, head or brain; without contrast material, followed by contrast material[s] and further sections), the provider rendering the service may substitute and render procedure code 70450 (Computed tomography, head or brain; without contrast material) or 70460 (Computed tomography, head or brain; with contrast material[s]). This would be considered "downcoding."
If other changes in procedure codes are necessary, such as an "upcode" or change in imaging modality, the provider who renders the service is required to contact eviCore healthcare to amend the PA request. Providers should be aware that PA amendments require approval from eviCore healthcare. Providers are strongly encouraged to obtain approval for a PA amendment prior to rendering services when possible.
Providers are encouraged to review approved PA requests before rendering the service to confirm the procedure code(s) authorized and confirm the assigned grant and expiration dates. Topic #10698 Communicating Prior Authorization Decisions
eviCore healthcare notifies the provider who submitted the PA request for advanced imaging services by fax whether a PA request is approved, approved with modifications, or denied. Providers should note that all PA communication is sent via fax from eviCore healthcare. Providers will not receive PA communications for PA requests for advanced imaging services in the mail unless eviCore healthcare is unable to send a fax (e.g., fax number is disconnected).
The provider who submitted the PA request receives a PA confirmation fax when a PA request is approved. The PA confirmation fax includes information about the procedure codes that are approved for the member and the grant (effective) and expiration dates for the PA.
The provider who submitted the PA request receives a PA confirmation fax and a PA decision notice letter when a PA request is approved with modifications. Prior authorization decision notice letters are sent via fax.
The provider who submitted the PA request receives a PA decision notice letter via fax when a PA request is denied.
Ordering providers are strongly encouraged to contact the provider who is rendering the service with information about the PA determination. The provider who renders the service is strongly encouraged to verify which services and procedure codes are authorized for the member by using the eviCore healthcare Portal or by contacting the ordering provider prior to rendering services.
The provider who renders the service will not automatically receive separate notification from eviCore healthcare regarding PA approvals, modifications, or denials, except in cases where the provider who renders the service submitted the original PA request. Topic #10699 Denied Requests
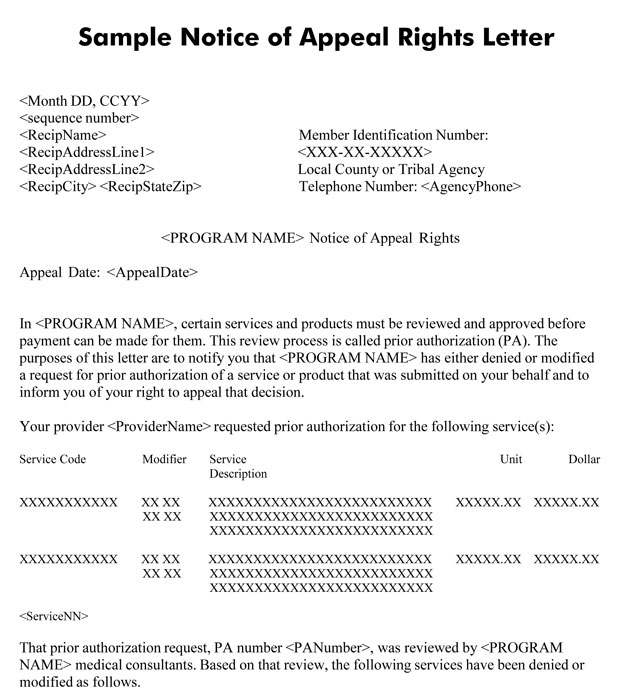
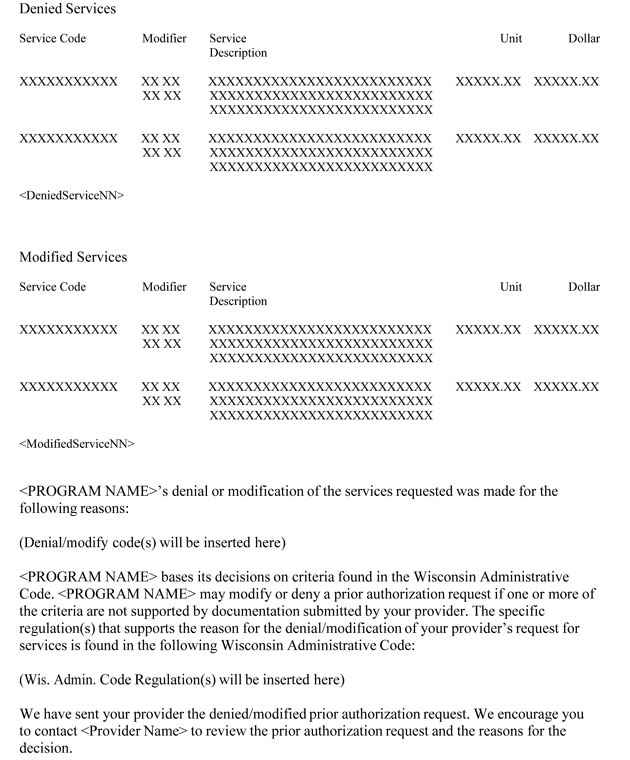
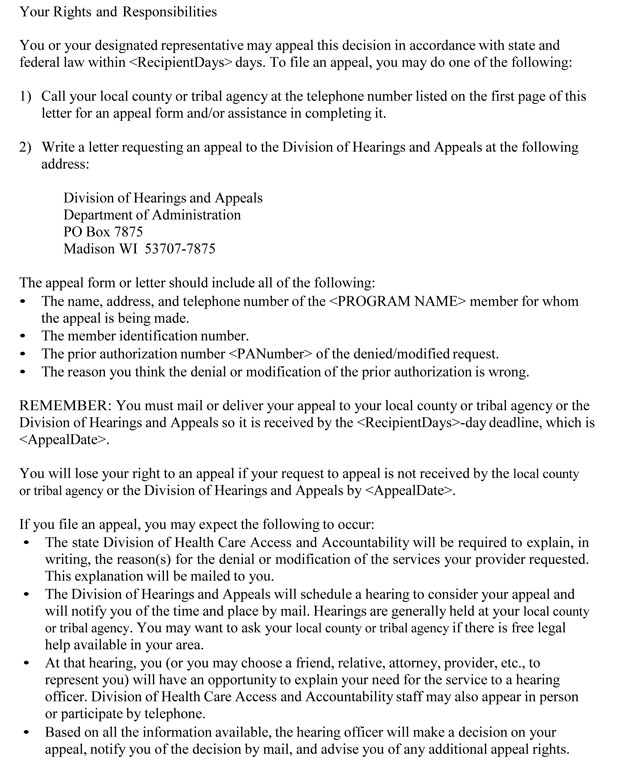
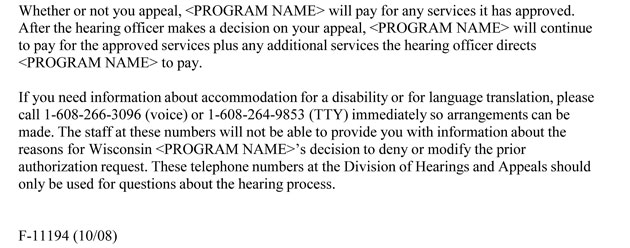
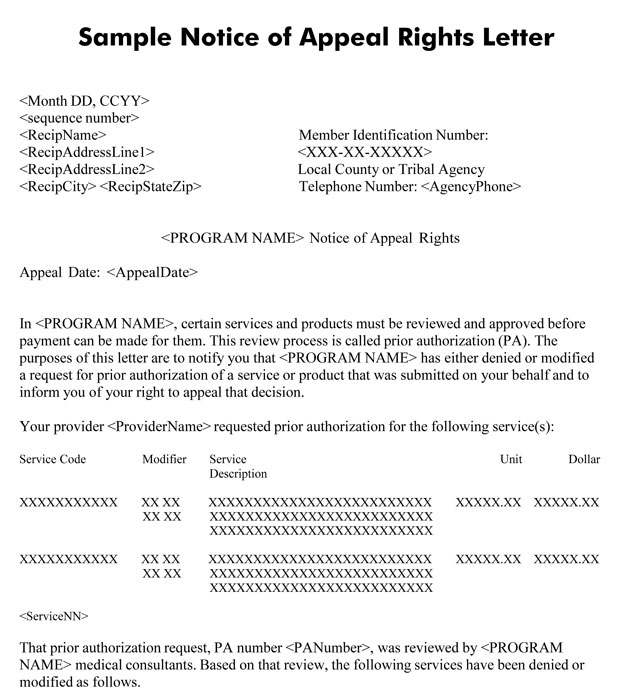
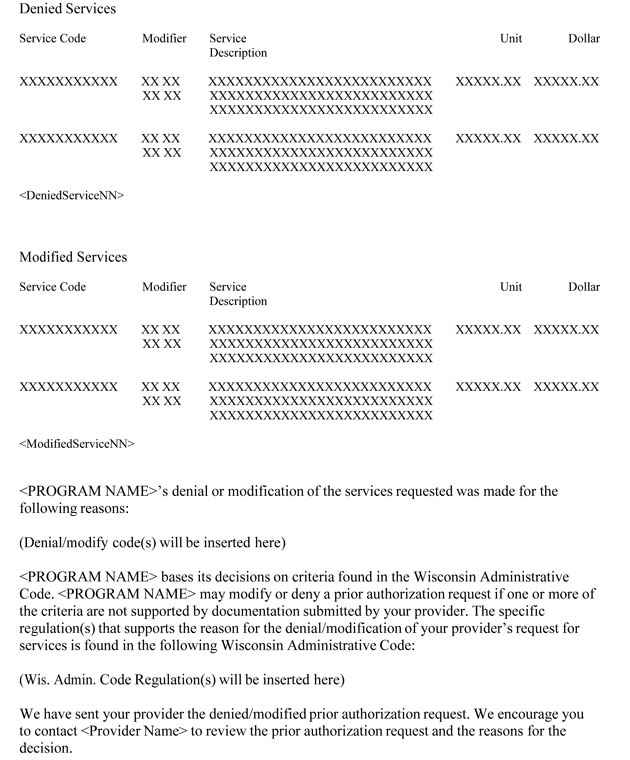
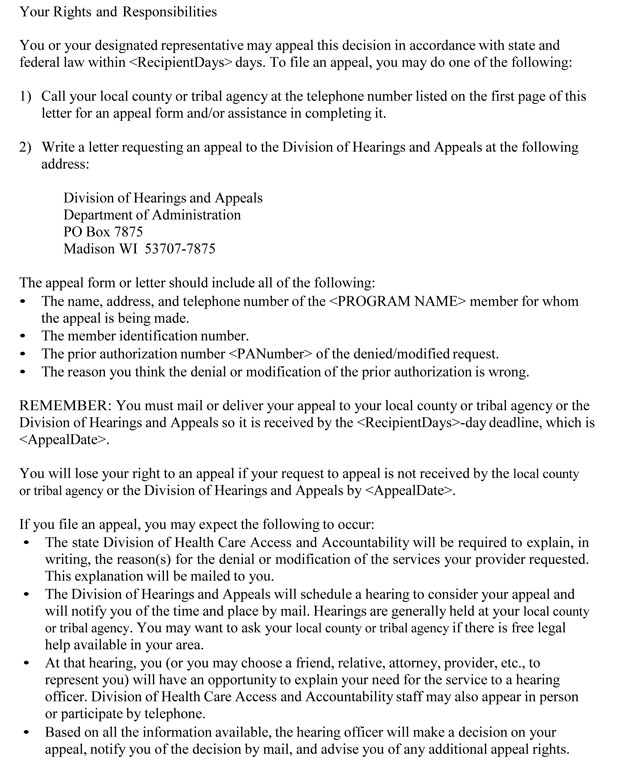
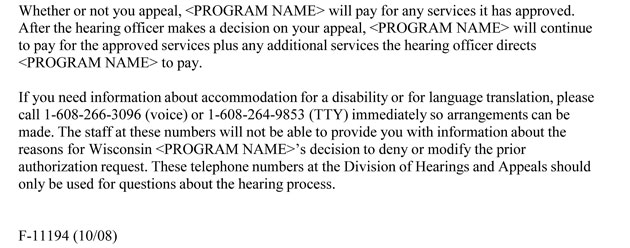
When a PA request for advanced imaging services is denied, both the provider who submitted the PA request and the member are notified. The provider receives a PA decision notice letter via fax that includes the reason for PA denial. The member receives a Notice of Appeal Rights letter that includes a brief statement of the reason PA was denied and information about their right to a fair hearing. Only the member, or authorized person acting on behalf of the member, can appeal the denial.
Providers may call eviCore healthcare for clarification of why a PA request was denied.
The provider who requested the PA is required to discuss a denied PA request with the member and is encouraged to help the member understand the reason the PA request was denied.
Providers have the following options when a PA request is denied:
- The provider who submitted the PA request may contact eviCore healthcare and request a
reconsideration for the denied service(s). (This is only an option for PA requests for advanced imaging services and not for other services that require PA under ForwardHealth policy.)
- The ordering provider or the provider who is to render the service may submit a new PA request.
- The provider who was to render the service may choose to not provide the service.
- The provider who renders the service may provide the service as a noncovered service.
If the member does not appeal the decision to deny the PA request or appeals the decision but the decision to deny the PA request is upheld, the member may choose to receive the originally requested service(s) as a noncovered service and to be responsible for payment.
 Topic #10700 Modified Requests
Modification is a change in the services originally requested on a PA request. Modifications include a partial approval (part of the service is approved and part of the service is denied) or the authorization of a procedure code(s) different than the one(s) originally requested.
Prior to modifying the PA request for advanced imaging services to authorize a different procedure code, eviCore healthcare contacts the provider who submitted the PA request by telephone. The provider must agree to the change in procedure code before the PA request can be approved. If the provider does not agree to the change, the PA request is denied.
When a PA request is modified, both the provider who submitted the PA request and the member are notified. The provider will be sent both a PA confirmation fax and a PA decision notice letter via fax that includes the reason the PA was modified. Ordering providers are encouraged to share the information on the PA confirmation fax and the PA decision notice letter with the provider who renders the service. The member receives a Notice of Appeal Rights letter that includes a brief statement of the reason the PA was modified and information on their right to a fair hearing. Only the member, or authorized person acting on behalf of the member, can appeal the modification.
Providers may call eviCore healthcare for clarification of why a PA request was modified.
The provider who requested the PA is required to discuss with the member the reason a PA request was modified and is encouraged to help the member understand the reason the PA request was modified.
Providers have the following options when a PA request is approved with modification:
- The provider who submitted the PA request may contact eviCore healthcare and request a
reconsideration for the denied service(s). (This is only an option for PA requests for advanced imaging services and not for other services that require PA under ForwardHealth policy.)
- The provider who renders the service may provide the service as authorized.
- The provider who was to render the service may choose to not provide the service.
- The provider who renders the service may provide the service as originally requested as a noncovered service.
If the member does not appeal the decision to modify the PA request or appeals the decision but the decision to modify the PA request is upheld, the member may choose to receive the service(s) originally requested as a noncovered service and be responsible for payment.
 |