| Program Name: | BadgerCare Plus and Medicaid | Handbook Area: | In-Home Mental Health/Substance Abuse Treatment Services for Children, HealthCheck "Other Services" | | 05/09/2024 | Prior Authorization : Forms and AttachmentsTopic #960 An Overview
Depending on the service being requested, most PA requests must be comprised of the following:
Topic #446 Attachments
In addition to the PA/RF, PA/HIAS1, or PA/DRF, a service-specific PA attachment must be submitted with each PA request. The PA attachment allows a provider to document the clinical information used to determine whether or not the standards of medical necessity are met for the requested service(s). Providers should include adequate information for ForwardHealth to make a reasonable judgment about the case.
ForwardHealth will scan each form with a barcode as it is received, which will allow greater efficiencies for processing PA requests. Topic #7489 Intensive In-Home Mental Health and Substance Abuse Treatment Services for Children
All intensive in-home mental health and substance abuse treatment services for children require PA before initiation of services. To request PA for intensive in-home mental health and substance abuse treatment services for children, providers will need to submit the following completed forms and required documentation to ForwardHealth:
- A PA/RF.
- PA/ITA.
- Physician's prescription or order signed and dated not more than one year prior to the requested first DOS.
- Current assessment and treatment plans. Providers may use their own assessment and treatment plan forms as long as all elements are included, or they may use the Prior Authorization Intensive In-Home Mental Health/Substance Abuse Services Assessment and Recovery/Treatment Plan Attachment, which includes the assessment, the multi-agency treatment plan, and the in-home recovery/treatment plan. Both a multi-agency treatment plan and an in-home treatment plan are required. These plans may be combined, making sure all required elements are included.
- The CANS assessment summary, the Achenbach Child Behavior Checklist, or the CAFAS.
Services are authorized based on the clinical documentation supplied by the provider. Services cannot be authorized earlier than the date of the prescription or order.
Information on backdating is available.
Assessment
Additional policy regarding the assessment includes the following:
- The assessment shall be sufficient to identify the member's need for intensive in-home services. A comprehensive assessment shall be valid; accurately reflect the member's current needs, strengths, and functioning as well as historical psychological, social, and physiological data, past treatment and outcome; and include necessary consultation to clarify the diagnosis and treatment.
- A substance abuse assessment must be included if substance abuse-related programming is part of the member's treatment program.
- Initial treatment goals may include assessment of the member and family in the home and these goals may be procedural (for example, complete assessment, complete substance abuse assessment). Where an assessment is part of the initial intervention, be specific and detailed as to the components of the assessment (for example, psychiatrist will complete psychiatric evaluation, substance abuse counselor will complete substance abuse assessment) and when the assessment will be completed. Where appropriate, identify any standardized assessment tools that will be utilized.
In-Home Recovery/Treatment Plan
Additional policy regarding the in-home recovery/treatment plan includes the following:
- The plan must contain measurable goals, specific methods, and an expected time frame for achievement of the goals. The methods must allow for a clear determination that the services provided meet criteria for covered services.
- The plan should clearly identify which team members are providing the services being requested.
- Services provided in the school, or that are primarily social or recreational in nature, are not reimbursable.
Multi-Agency Treatment Plan
Additional policy regarding the multi-agency treatment plan includes the following:
- The individual who is coordinating the multi-agency planning should be clearly identified.
- The multi-agency treatment plan must be developed by representatives from all systems identified on the severe emotional disturbance eligibility checklist.
- The plan should be signed by all participants, but to facilitate submission, the provider may document who was involved.
- Where an agency was not involved in the planning, the provider is required to document the reason and what attempts were made to include them.
- The plan must address the role of each system in the overall treatment and the major goals for each agency involved.
Child and Adolescent Needs and Strengths Assessment Summary, Achenbach Child Behavior Checklist, and the Child and Adolescent Functional Assessment Scale
Providers are required to complete and attach the results of the CANS assessment summary, Achenbach Child Behavior Checklist, or the CAFAS.
Providers are required to be trained to use the CANS assessment tool. For information on how to obtain the CANS assessment tool or training, providers should contact Provider Services.
Information about these screening instruments is available on the internet by searching for "Child and Adolescent Needs and Strengths assessment summary," "Achenbach Behavior Checklist," or "Child and Adolescent Functional Assessment Scale." Topic #447 Obtaining Forms and Attachments
Providers may obtain paper versions of all PA forms and attachments. In addition, providers may download and complete most PA attachments from the ForwardHealth Portal.
Paper Forms
Paper versions of all PA forms and PA attachments are available by writing to ForwardHealth. Include a return address, the name of the form, the form number (if applicable), and mail the request to the following address:
ForwardHealth
Form Reorder
313 Blettner Blvd
Madison WI 53784
Providers may also call Provider Services to order paper copies of forms.
Downloadable Forms
Most PA attachments can be downloaded and printed in their original format from the Portal. Many forms are available in fillable PDF and fillable Microsoft Word formats.
Web PA Via the Portal
Certain providers may complete the PA/RF and PA attachments through the Portal. Providers may then print the PA/RF (and in some cases the PA attachment), and send the PA/RF, service-specific PA attachments, and any supporting documentation on paper by mail or fax to ForwardHealth. Topic #448 Prior Authorization Request Form
The PA/RF is used by ForwardHealth and is mandatory for most providers when requesting PA. The PA/RF serves as the cover page of a PA request.
Providers are required to complete the basic provider, member, and service information on the PA/RF. Each PA request is assigned a unique ten-digit number. ForwardHealth remittance information will report to the provider the PA number used to process the claim for prior authorized services. Topic #7481 Prior Authorization Request Form Completion Instructions for Intensive In-Home Mental Health and Substance Abuse Treatment Services for Children
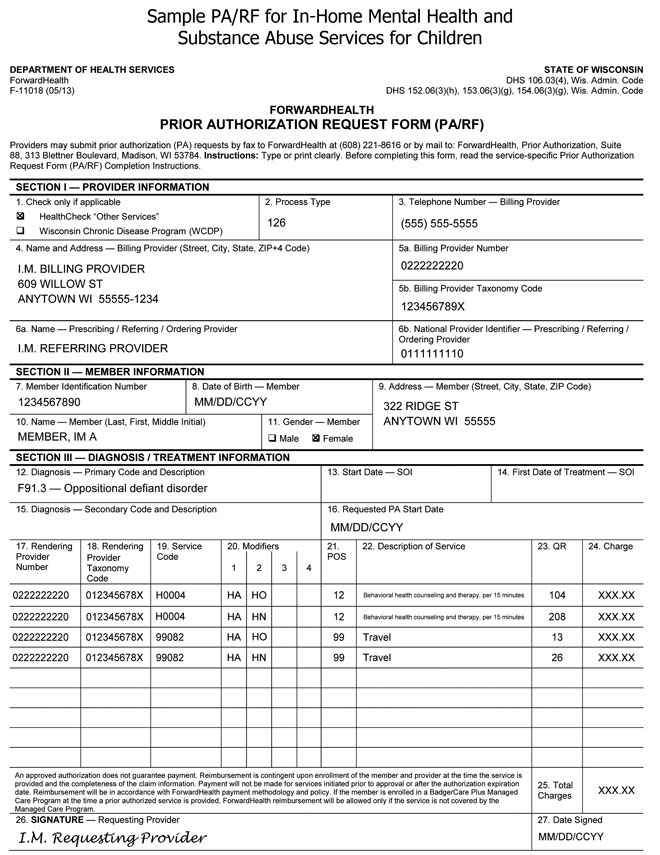
A sample PA/RF for intensive in-home mental health and substance abuse treatment services for children is available.
ForwardHealth requires certain information to enable the programs to authorize and pay for medical services provided to eligible members.
Members of ForwardHealth are required to give providers full, correct, and truthful information for the submission of correct and complete claims for reimbursement. This information should include, but is not limited to, information concerning enrollment status, accurate name, address, and member identification number (Wis. Admin. Code § DHS 104.02[4]).
Under Wis. Stat. § 49.45(4), personally identifiable information about program applicants and members is confidential and is used for purposes directly related to ForwardHealth administration such as determining eligibility of the applicant, processing PA requests, or processing provider claims for reimbursement. The use of the PA/RF is mandatory to receive PA for certain items. Failure to supply the information requested by the form may result in denial of PA or payment for the service.
Providers should make duplicate copies of all paper documents mailed to ForwardHealth. Providers may submit PA requests, along with the PA/ITA, by fax to ForwardHealth at 608-221-8616 or by mail to the following address:
ForwardHealth
Prior Authorization
Ste 88
313 Blettner Blvd
Madison WI 53784
The provision of services that are greater than or significantly different from those authorized may result in nonpayment of the billing claim(s).
SECTION I ― PROVIDER INFORMATION
Element 1 — HealthCheck "Other Services" and Wisconsin Chronic Disease Program (WCDP)
Enter an "X" in the box next to HealthCheck "Other Services" if the services requested on the PA/RF are for HealthCheck "Other Services." Enter an "X" in the box next to WCDP if the services requested on the PA/RF are for a WCDP member.
Element 2 — Process Type
Enter processing type "126" — Psychotherapy.
Element 3 — Telephone Number — Billing Provider
Enter the phone number, including the area code, of the office, clinic, facility, or place of business of the billing provider.
Element 4 — Name and Address — Billing Provider
Enter the name and complete address (street, city, state, and ZIP+4 code) of the billing provider. Providers are required to include both the ZIP code and four-digit extension for timely and accurate billing. The name listed in this element must correspond with the billing provider number listed in Element 5a.
Element 5a — Billing Provider Number
Enter the NPI of the billing provider. The NPI in this element must correspond with the provider name listed in Element 4.
Element 5b — Billing Provider Taxonomy Code
Enter the national 10-digit alphanumeric taxonomy code that corresponds to the NPI of the billing provider in Element 5a.
Element 6a — Name — Prescribing/Referring/Ordering Provider
Enter the prescribing/referring/ordering provider's name.
Element 6b — National Provider Identifier — Prescribing/Referring/Ordering Provider
Enter the prescribing/referring/ordering provider's 10-digit NPI.
SECTION II ― MEMBER INFORMATION
Element 7 — Member Identification Number
Enter the member ID. Do not enter any other numbers or letters. Use the ForwardHealth identification card or Wisconsin's EVS to obtain the correct number.
Element 8 — Date of Birth — Member
Enter the member's date of birth in mm/dd/ccyy format.
Element 9 — Address — Member
Enter the complete address of the member's place of residence, including the street, city, state, and ZIP code. If the member is a resident of a nursing home or other facility, include the name of the nursing home or facility.
Element 10 — Name — Member
Enter the member's last name, followed by their first name and middle initial. Use the EVS to obtain the correct spelling of the member's name. If the name or spelling of the name on the ForwardHealth card and the EVS do not match, use the spelling from the EVS.
Element 11 — Gender — Member
Enter an "X" in the appropriate box to specify male or female.
SECTION III ― DIAGNOSIS / TREATMENT INFORMATION
Element 12 — Diagnosis — Primary Code and Description
Enter the appropriate ICD diagnosis code and description with the highest level of specificity most relevant to the service/procedure requested. The ICD diagnosis code must correspond with the ICD description.
Element 13 — Start Date — SOI (not required)
Element 14 — First Date of Treatment — SOI (not required)
Element 15 — Diagnosis — Secondary Code and Description
Enter the appropriate secondary ICD diagnosis code and description with the highest level of specificity most relevant to the service/procedure requested, if applicable. The ICD diagnosis code must correspond with the ICD description.
Element 16 — Requested PA Start Date
Enter the requested start date for service(s) in mm/dd/ccyy format, if a specific start date is requested. If backdating is requested, include the clinical rationale for starting before PA was received. Backdating is not allowed on subsequent PA requests.The maximum backdating allowed is 10 working days from the date of receipt from ForwardHealth.
Element 17 — Rendering Provider Number
Enter the NPI of the Medicaid-enrolled psychotherapist or Medicaid-enrolled substance abuse counselor.
Element 18 — Rendering Provider Taxonomy Code
Enter the national 10-digit alphanumeric taxonomy code of the Medicaid-enrolled psychotherapist or Medicaid-enrolled substance abuse counselor.
Element 19 — Service Code
Enter the appropriate procedure code for each service requested.
Element 20 — Modifiers
Enter the modifier(s) corresponding to the service code listed if a modifier is required.
Element 21 — POS
Enter the appropriate POS code designating where the requested service would be provided.
Element 22 — Description of Service
Enter a written description corresponding to the appropriate procedure code for services.
Element 23 — QR
Enter the appropriate quantity (for example, number of services, days' supply) requested for the procedure code listed. Refer to the available rounding guidelines.
Element 24 — Charge
Enter the provider's usual and customary charge for each service/procedure/item requested. If the quantity is greater than "1.0," multiply the quantity by the charge for each service/procedure/item requested. Enter the total amount in this element.
Note: The charges indicated on the request form should reflect the provider's usual and customary charge for the procedure requested. Providers are reimbursed for authorized services according to provider terms of reimbursement issued by the Wisconsin DHS.
Element 25 — Total Charges
Enter the anticipated total charges for this request.
Element 26 — Signature — Requesting Provider
The original signature of the provider requesting/performing/dispensing this service/procedure/item must appear in this element.
Element 27 — Date Signed
Enter the month, day, and year the PA/RF was signed (in mm/dd/ccyy format).
 Topic #449 Supporting Clinical Documentation
Certain PA requests may require additional supporting clinical documentation to justify the medical necessity for a service(s). Supporting documentation may include, but is not limited to, X-rays, photographs, a physician's prescription, clinical reports, and other materials related to the member's condition.
All supporting documentation submitted with a PA request must be clearly labeled and identified with the member's name and member identification number. Securely packaged X-rays and dental models will be returned to providers.
Photographs submitted to ForwardHealth as additional supporting clinical documentation for PA requests will not be returned to providers and will be disposed of securely. Topic #3759 Utilizing Medical Record Documentation
Providers may submit selected existing medical documentation with a PA request in lieu of writing the same required information on the PA attachment.
For example, as supportive documentation, the current treatment plan could be attached rather than rewritten on the PA attachment. In this case, the provider should write, "See attached treatment plan dated MM/DD/YY" in the element requesting the current treatment plan on the PA attachment. |