| Program Name: | BadgerCare Plus and Medicaid | Handbook Area: | Specialized Medical Vehicle | | 07/14/2025 | Claims : SubmissionTopic #17797 1500 Health Insurance Claim Form Completion Instructions
These instructions are for the completion of the 1500 Health Insurance Claim Form for ForwardHealth. Refer to the
1500 Health Insurance Claim Form Reference Instruction Manual for Form Version 02/12,
prepared by the NUCC and available on their website, to view instructions for all item numbers not listed below.
Use the following claim form completion instructions, in conjunction with the 1500 Health Insurance Claim Form Reference Instruction Manual for Form Version 02/12, prepared by the NUCC, to avoid denial
or inaccurate claim payment. Be advised that every code used is required to be a valid code, even if it is entered in a non-required field. Do not include attachments unless instructed to do so.
Members enrolled in BadgerCare Plus or Medicaid receive a ForwardHealth member identification card. Always verify a member's enrollment before providing nonemergency services to determine if there are
any limitations to covered services and to obtain the correct spelling of the member's name.
When submitting a claim with multiple pages, providers are required to indicate page numbers using the format "Page X of X" in the upper right corner of the claim form.
Other health insurance sources must be billed prior to submitting claims to ForwardHealth, unless the service does not require commercial health
insurance billing as determined by ForwardHealth. When submitting paper claims, if the member has any other health insurance sources, providers are required to complete and submit an Explanation of Medical Benefits form, along with the completed paper claim.
Submit completed paper claims and the completed Explanation of Medical Benefits form, as applicable, to the following address:
ForwardHealth
Claims and Adjustments
313 Blettner Blvd
Madison WI 53784
Item Number 6 — Patient Relationship to Insured
Enter "X" in the "Self" box to indicate the member's relationship to insured when Item Number 4 is completed. Only one box can be marked.
Item Number 9 — Other Insured's Name (not required)
This field is not required on the claim.
Note: When submitting paper claims to ForwardHealth, if the member has any other health insurance sources (for example, commercial health insurance, Medicare, Medicare Advantage Plans), providers are required to complete and submit a separate Explanation of Medical Benefits form for each other payer as an attachment(s) to their completed paper claim.
Item Number 9a — Other Insured's Policy or Group Number (not required)
This field is not required on the claim.
Note: When submitting paper claims to ForwardHealth, if the member has any other health insurance sources (for example, commercial health insurance, Medicare, Medicare Advantage Plans), providers are required to complete and submit a separate Explanation of Medical Benefits form for each other payer as an attachment(s) to their completed paper claim.
Item Number 9d — Insurance Plan Name or Program Name (not required)
This field is not required on the claim.
Note: When submitting paper claims to ForwardHealth, if the member has any other health insurance sources (for example, commercial health insurance, Medicare, Medicare Advantage Plans), providers are required to complete and submit a separate Explanation of Medical Benefits form for each other payer as an attachment(s) to their completed paper claim.
Item Number 10d — Claim Codes (Designated by NUCC)
When applicable, enter the Condition Code. The Condition Codes approved for use on the 1500 Health Insurance Claim Form are available on the
NUCC website under Code Sets.
Item Number 11 — Insured's Policy Group or FECA Number (not required)
This field is not required on the claim.
Note: When submitting paper claims to ForwardHealth, if the member has any other health insurance sources (for example, commercial health insurance, Medicare, Medicare Advantage Plans), providers are required to complete and submit a separate Explanation of Medical Benefits form for each other payer as an attachment(s) to their completed paper claim.
Item Number 11d — Is There Another Health Benefit Plan?
This field is not used for processing by ForwardHealth.
Item Number 19 — Additional Claim Information (Designated by NUCC)
When applicable, enter provider identifiers or taxonomy codes. A list of applicable qualifiers are defined by the NUCC and can be found in the NUCC 1500 Health Insurance Claim Form Reference
Instruction Manual for Form Version 02/12, prepared by the NUCC.
If a provider bills an unlisted (or not otherwise classified) procedure code, a description of the
procedure must be indicated in this field. If a more specific code is not available, the provider is required to submit the appropriate documentation, which could include a PA request, to justify use of the unlisted procedure code and to describe the procedure or service rendered.
Item Number 22 — Resubmission Code and/or Original Reference Number
This field is not used for processing by ForwardHealth.
Section 24
The six service lines in section 24 have been divided horizontally. Enter service information in the bottom, unshaded area of the six service lines. The horizontal division of each service line is not
intended to allow the billing of 12 lines of service.
For physician-administered drugs: NDCs must be indicated in the shaded area of Item Numbers 24A-24G. Each NDC must be accompanied by an NDC qualifier, unit
qualifier, and units. To indicate an NDC, providers should do the following:
- Indicate the NDC qualifier N4, followed by the 11-digit NDC, with no space in between.
- Indicate one space between the NDC and the unit qualifier.
- Indicate one unit qualifier (F2 [International unit], GR [Gram], ME [Milligram], ML [Milliliter], or UN [Unit]), followed by the NDC units, with no space in between.
For additional information about submitting a 1500 Health Insurance Claim Form with supplemental NDC information, refer to the completion instructions located under "Section 24" in the Field Specific
Instructions section of the NUCC's 1500 Health Insurance Claim Form Reference Instruction Manual for Form Version 02/12.
Item Number 24C — EMG
Enter a "Y" in the unshaded area for each procedure performed as an emergency. If the procedure was not an emergency, leave this field blank.
Item Number 29 — Amount Paid (not required)
This field is not required on the claim.
Note: When submitting paper claims to ForwardHealth, if the member has any other health insurance sources (for example, commercial health insurance, Medicare, Medicare Advantage Plans), providers are required to complete and submit a separate Explanation of Medical Benefits form for each other payer as an attachment(s) to their completed paper claim. Topic #542 Attached Documentation
Providers should not submit additional documentation with a claim unless specifically requested. Topic #15737 Claims for Services Prescribed, Referred, or Ordered
Claims for services that are prescribed, referred, or ordered services must include the
Type 1
NPI of the Medicaid-enrolled provider who prescribed, referred, or ordered the service. ForwardHealth will deny claims if they do not include a Medicaid-enrolled provider's NPI or if they are submitted with the NPI of a provider who is not enrolled with Wisconsin Medicaid. (However, providers should not include the NPI of a provider who prescribes, refers, or orders services on claims for services that are not prescribed, referred, or ordered, as those claims will also deny if the provider is not enrolled in Medicaid.)
Note: Claims submitted for ESRD services do not require referring provider information; however, prescribing and ordering provider information will still be required on claims.
Contacting Prescribing/Referring/Ordering Provider After a Claim Denial
If a claim is denied for prescribed, referred, or ordered services because the prescribing/referring/ordering provider was not Medicaid-enrolled, the rendering provider should contact the prescribing/referring/ordering provider and:
- Communicate that the prescribing/referring/ordering provider is must be enrolled in Wisconsin Medicaid.
- Inform the prescribing/referring/ordering provider of the limited enrollment available for prescribing/referring/ordering providers.
- Resubmit the claim once the prescribing/referring/ordering provider has enrolled in Wisconsin Medicaid.
Exception for Prescribed, Referred, or Ordered Services Prior to a Member's Medicaid Enrollment
Providers may submit claims for prescribed, referred, or ordered services by a non-Medicaid-enrolled provider if the member was not yet enrolled in Wisconsin Medicaid at the time the prescription, referral, or order was written (and the member has since enrolled in Wisconsin Medicaid). However, once the prescription, referral, or order expires, the prescribing/referring/ordering provider is required to enroll in Wisconsin Medicaid if they continue to prescribe, refer, or order services for the member.
The procedures for submitting claims for this exception depend on the type of claim submitted:
- Institutional, professional, and dental claims for this exception must be sent to the following address:
ForwardHealth
P.R.O. Exception Requests
Ste 50
313 Blettner Blvd
Madison WI 53784
A copy of the prescription, referral, or order must be included with the claim.
- Pharmacy and compound claims for this exception do not require any special handling. These claims include a prescription date, so they can be processed to bypass the prescriber Medicaid enrollment requirement in situations where the provider prescribed services before the member was enrolled in Wisconsin Medicaid.
Topic #6957 Copy Claims on the ForwardHealth Portal
Providers can copy institutional, professional, and dental paid claims on the ForwardHealth Portal. Providers can open any paid claim, click the "Copy" button, and all of the information on the claim will be copied over to a new claim form. Providers can then make any desired changes to the claim form and click "Submit" to submit as a new claim. After submission, ForwardHealth will issue a response with a new ICN along with the claim status. Topic #5017 Correct Errors on Claims and Resubmit to ForwardHealth on the Portal
Providers can view EOB codes and descriptions for any claim submitted to ForwardHealth on the ForwardHealth Portal. The EOBs help providers determine why a claim did not process successfully, so providers may correct the error online and resubmit the claim. The EOB appears on the bottom of the screen and references the applicable claim header or detail. Topic #4997 Direct Data Entry of Professional and Institutional Claims on the Portal
Providers can submit the following claims to ForwardHealth via DDE on the ForwardHealth Portal:
- Professional claims
- Institutional claims
- Dental claims
- Compound drug claims
- Noncompound drug claims
DDE is an online application that allows providers to submit claims directly to ForwardHealth.
When submitting claims via DDE, required fields are indicated with an asterisk next to the field. If a required field is left blank, the claim will not be submitted, and a message will appear prompting the provider to complete the specific required field(s). Portal help is available for each online application screen. In addition, search functions accompany certain fields so providers do not need to look up the following information in secondary resources.
On professional claim forms, providers may search for and select the following:
- Procedure codes
- Modifiers
- Diagnosis codes
- Place of service codes
On institutional claim forms, providers may search for and select the following:
- Type of bill
- Patient status
- Visit point of origin
- Visit priority
- Diagnosis codes
- Revenue codes
- Procedure codes
- HIPPS codes
- Modifiers
On dental claims, providers may search for and select the following:
- Procedure codes
- Rendering providers
- Area of the oral cavity
- Place of service codes
On compound and noncompound drug claims, providers may search for and select the following:
- Diagnosis codes
- NDCs
- Place of service codes
- Professional service codes
- Reason for service codes
- Result of service codes
Using DDE, providers may submit claims for compound drugs and single-entity drugs. Any provider, including a provider of DME or of DMS who submits noncompound drug claims, may submit these claims via DDE. All claims, including POS claims, are viewable via DDE. Topic #344 Electronic Claim Submission
Providers are encouraged to submit claims electronically. Electronic claim submission does the following:
- Adapts to existing systems
- Allows flexible submission methods
- Improves cash flow
- Offers efficient and timely payments
- Reduces billing and processing errors
- Reduces clerical effort
Topic #1818 Electronic Claim Submission for Specialized Medical Vehicle Services
SMV providers are required to receive Wisconsin DHS approval before they may use electronic claims submission. DHS requires that all SMV providers be audited before receiving this approval. Once an audit is completed, providers receive a letter from the DHS notifying them whether or not they are eligible to begin electronic claims submission. If providers are eligible, the letter will contain instructions on how to proceed setting up electronic claims submission.
Providers are encouraged to submit claims electronically if that option is available to them. Users may submit claims using PES software. To obtain PES software, providers may download it from the ForwardHealth Portal. For assistance installing and using PES software, providers may call the EDI Helpdesk. Topic #16937 Electronic Claims and Claim Adjustments With Other Commercial Health Insurance Information
Effective for claims and claim adjustments submitted electronically via the Portal or PES software on and after June 16, 2014, other insurance information must be submitted at the detail level on professional, institutional, and dental claims and adjustments if it was processed at the detail level by the primary insurance. Except for a few instances, Wisconsin Medicaid or BadgerCare Plus is the payer of last resort for any covered services; therefore, providers are required to make a reasonable effort to exhaust all existing other health insurance sources before submitting claims to ForwardHealth or to a state-contracted MCO.
Other insurance information that is submitted at the detail level via the Portal or PES software will be processed at the detail level by ForwardHealth.
Under HIPAA, claims and adjustments submitted using an 837 transaction must include detail-level information for other insurance if they were processed at the detail level by the primary insurance.
Adjustments to Claims Submitted Prior to June 16, 2014
Providers who submit professional, institutional, or dental claim adjustments electronically on and after June 16, 2014, for claims originally submitted prior to June 16, 2014, are required to submit other insurance information at the detail level on the adjustment if it was processed at the detail level by the primary insurance. Topic #365 Extraordinary Claims
Extraordinary claims are claims that have been denied by a BadgerCare Plus HMO or SSI HMO and should be submitted to fee-for-service. Topic #4837 HIPAA-Compliant Data Requirements
Procedure Codes
All fields submitted on paper and electronic claims are edited to ensure HIPAA compliance before being processed. Compliant code sets include CPT and HCPCS procedure codes entered into all fields, including those fields that are Not Required or Optional.
If the information in all fields is not valid and recognized by ForwardHealth, the claim will be denied.
Provider Numbers
For health care providers, NPIs are required in all provider number fields on paper claims and 837 transactions, including rendering, billing, referring, prescribing, attending, and Other provider fields.
Non-healthcare providers, including personal care providers, SMV providers, blood banks, and CCOs should enter valid provider numbers into fields that require a provider number. Topic #562 Managed Care Organizations
Claims for services that are covered in a member's state-contracted MCO should be submitted to that MCO. Topic #10837 Note Field for Most Claims Submitted Electronically
In some instances, ForwardHealth requires providers to include a description of a service identified by an unlisted, or NOC, procedure code. Providers submitting claims electronically should include a description of an NOC procedure code in a Notes field, if required. The Notes field allows providers to enter up to 80 characters. In some cases, the Notes field allows providers to submit NOC procedure code information on a claim electronically instead of on a paper claim or with a paper attachment to an electronic claim.
The Notes field should only be used for NOC procedure codes that do not require PA.
Claims Submitted via the ForwardHealth Portal Direct Data Entry or Provider Electronic Solutions
A notes field is available on the ForwardHealth Portal DDE and PES software when providers submit the following types of claims:
- Professional
- Institutional
- Dental
On the professional form, the Notes field is available on each detail. On the institutional and dental forms, the Notes field is only available on the header.
Claims Submitted via 837 Health Care Claim Transactions
ForwardHealth accepts and utilizes information submitted by providers about NOC procedure codes in certain loops/segments on the 837 transactions. Refer to the companion guides for more information. Topic #561 Paper Claim Form Preparation and Data Alignment Requirements
Optical Character Recognition
Paper claims submitted to ForwardHealth on the 1500 Health Insurance Claim Form and UB-04 Claim Form are processed using OCR software that recognizes printed, alphanumeric text. OCR software increases efficiency by alleviating the need for keying in data from paper claims.
The data alignment requirements do not apply to the Compound Drug Claim form and the Noncompound Drug Claim form.
Speed and Accuracy of Claims Processing
OCR software processes claim forms by reading text within fields on claim forms. After a paper claim form is received by ForwardHealth, the claim form is scanned so that an image can be displayed
electronically. The OCR software reads the electronic image on file and populates the information into the ForwardHealth interChange system. This technology increases accuracy by removing the possibility of errors being made during manual keying.
OCR software speeds paper claim processing, but only if providers prepare their claim forms correctly. In order for OCR software to read the claim form accurately, the quality of copy and the alignment of text within individual fields on the claim form need to be precise. If data are misaligned, the claim could be processed incorrectly. If data cannot be read by the OCR software, the process will stop and the electronic image of the claim form will need to be reviewed and keyed manually. This will cause an increase in processing time.
Handwritten Claims
Submitting handwritten claims should be avoided whenever possible. ForwardHealth accepts handwritten claims; however, it is very difficult for OCR software to read a handwritten claim. If a handwritten claim cannot be read by the OCR software, it will need to be keyed manually from the electronic image of the claim form. Providers should avoid submitting claims
with handwritten corrections as this can also cause OCR software processing delays.
Use Original Claim Forms
Only original 1500 Health Insurance Claim Forms and UB-04 Claim Forms should
be submitted. Original claim forms are printed in red ink and may be obtained
from a federal forms supplier. ForwardHealth does not provide these claim forms.
Claims that are submitted as photocopies cannot be read by OCR software and will
need to be keyed manually from an electronic image of the claim form. This could
result in processing delays.
Use Laser or Ink Jet Printers
It is recommended that claims are printed using laser or ink jet printers
rather than printers that use DOT matrix. DOT matrix printers have breaks in the
letters and numbers, which may cause the OCR software to misread the claim form.
Use of old or worn ink cartridges should also be avoided. If the claim form is
read incorrectly by the OCR software, the claim may be denied or reimbursed
incorrectly. The process may also be stopped if it is unable to read the claim
form, which will cause a delay while it is manually reviewed.
Alignment
Alignment within each field on the claim form needs to be accurate. If text
within a field is aligned incorrectly, the OCR software may not recognize that
data are present within the field or may not read the data correctly. For
example, if a reimbursement amount of $300.00 is entered into a field on the
claim form, but the last "0" is not aligned within the field, the OCR software
may read the number as $30.00, and the claim will be reimbursed incorrectly.
To get the best alignment on the claim form, providers should center
information vertically within each field, and align all information on the same
horizontal plane. Avoid squeezing two lines of text into one of the six line
items on the 1500 Health Insurance Claim Form.
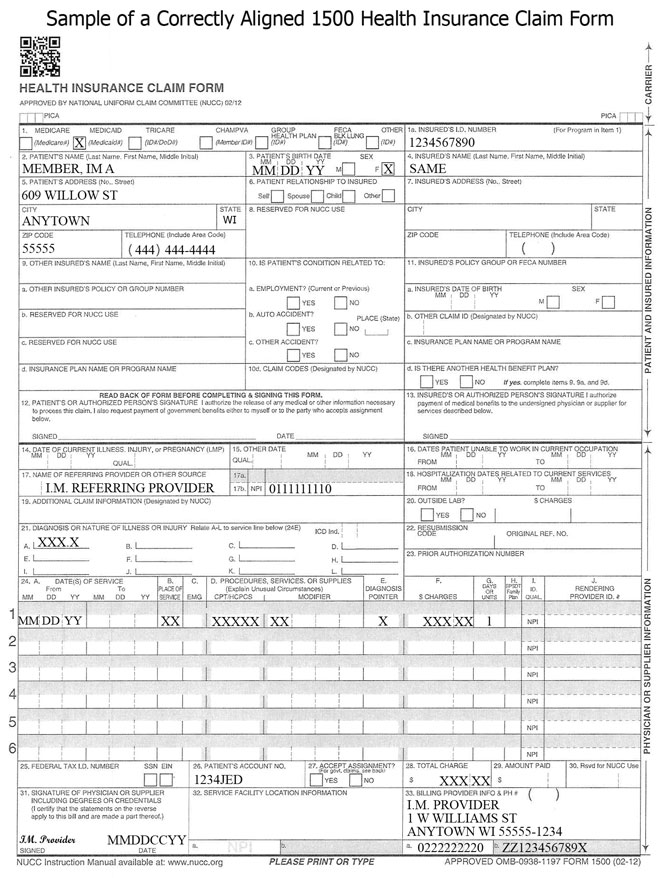
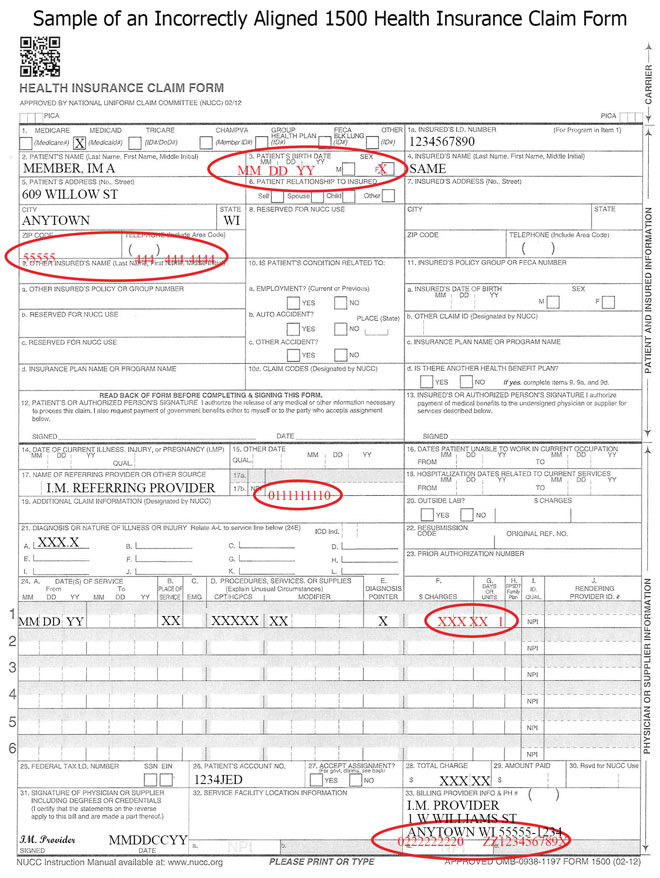
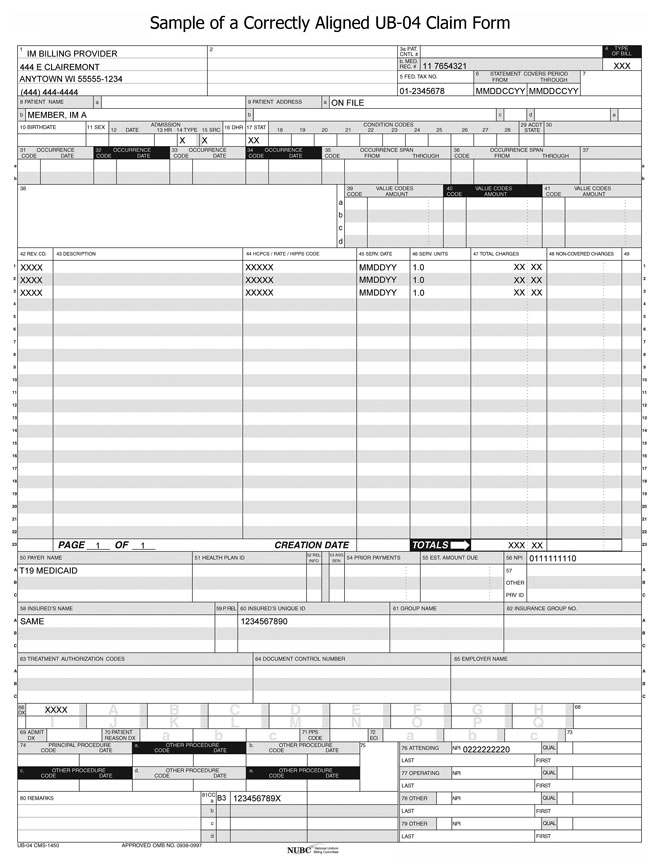
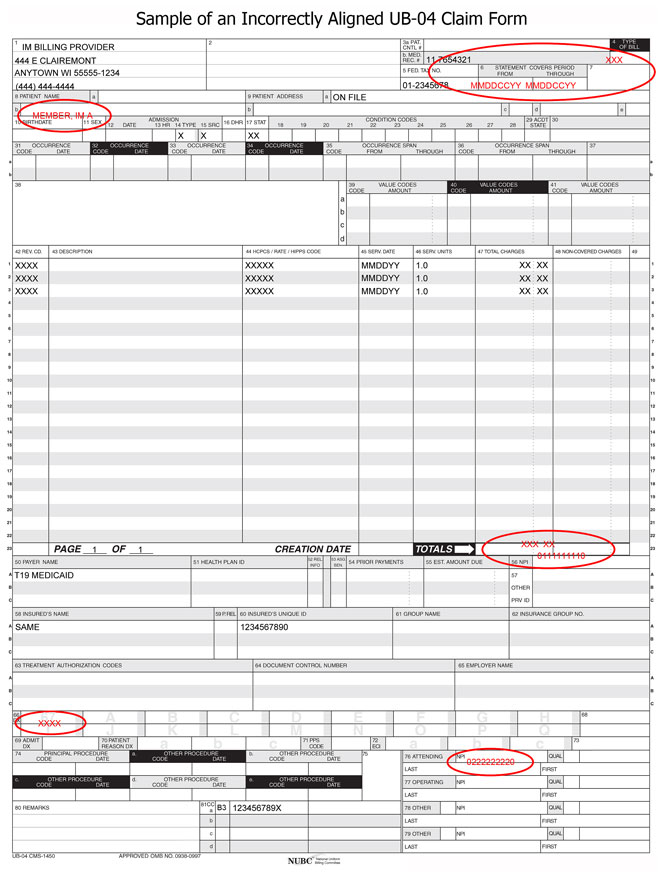
The following sample claim forms demonstrate correct and incorrect alignment:
Clarity
Clarity is very important. If information on the claim form is not clear
enough to be read by the OCR software, the process may stop, prompting manual
review.
The following guidelines will produce the clearest image and optimize
processing time:
- Use 10-point or 12-point Times New Roman or Courier New font.
- Type all claim data in uppercase letters.
- Use only black ink to complete the claim form.
- Avoid using italics, bold, or script.
- Make sure characters do not touch.
- Make sure there are no lines from the printer cartridge anywhere on the
claim form.
- Avoid using special characters such as dollar signs, decimals, dashes,
asterisks, or backslashes, unless it is specified that these characters should
be used.
- Use Xs in check boxes. Avoid using letters such as Y for Yes, N for
No, M for Male, or F for Female.
- Do not highlight any information on the claim form. Highlighted
information blackens when it is imaged, and the OCR software will be unable to
read it.
Note: The above guidelines will also produce the clearest image for
claims that need to be keyed manually from an electronic image.
Staples, Correction Liquid, and Correction Tape
The use of staples, correction liquid, correction tape, labels, or stickers
on claim forms should be avoided. Staples need to be removed from claim forms
before they can be imaged, which can damage the claim and cause a delay in
processing time. Correction liquid, correction tape, labels, and stickers can
cause data to be read incorrectly or cause the OCR process to stop, prompting
manual review. If the form cannot be read by the OCR software, it will need to
be keyed manually from an electronic image.
Additional Diagnosis Codes
ForwardHealth will accept up to 12 diagnosis codes in Item Number 21 of the
1500 Health Insurance Claim Form.
 Topic #1817 Paper Claim Submission
Paper claims for SMV services must be submitted using the 1500 Health Insurance Claim Form. Claims for SMV services submitted on any other claim form are denied.
Providers should use the appropriate claim form instructions for SMV services when submitting these claims.
Obtaining the Claim Forms
ForwardHealth does not provide the 1500 Health Insurance Claim Form. The form may be obtained from any federal forms supplier. Topic #22797 Payment Integrity Review Supporting Documentation
Providers are notified that an individual claim is subject to PIR through a message on the Portal when submitting claims. When this occurs, providers have seven calendar days to submit the supporting documentation that must be retained in the member's record for the specific service billed. This documentation must be attached to the claim. The following are examples of documentation providers may attach to the claim; however, this list is not exhaustive, and providers may submit any documentation available to substantiate payment:
- Case management or consultation notes
- Durable medical equipment or supply delivery receipts or proof of delivery and itemized invoices or bills
- Face-to-face encounter documentation
- Individualized plans of care and updates
- Initial or program assessments and questionnaires to indicate the start DOS
- Office visit documentation
- Operative reports
- Prescriptions or test orders
- Session or service notice for each DOS
- Testing and lab results
- Transportation logs
- Treatment notes
Providers must attach this documentation to the claim at the time of, or up to seven days following, submission of the claim. A claim may be denied if the supporting documentation is not submitted. If a claim is denied, providers may submit a new claim with the required documentation for reconsideration. To reduce provider impact, claims reviewed by the OIG will be processed as quickly as possible, with an expected average adjudication of 30 days. Topic #4817 Submitting Paper Attachments With Electronic Claims
Providers may submit paper attachments to accompany electronic claims and electronic claim adjustments. Providers should refer to their companion guides for directions on indicating that a paper attachment will be submitted by mail.
Paper attachments that go with electronic claim transactions must be submitted with the Claim Form Attachment Cover Page. Providers are required to indicate an ACN for paper attachment(s) submitted with electronic claims. (The ACN is an alphanumeric entry between two and 80 digits assigned by the provider to identify the attachment.) The ACN must be indicated on the cover page so that ForwardHealth can match the paper attachment(s) to the correct electronic claim.
ForwardHealth will hold an electronic claim transaction or a paper attachment(s) for up to seven calendar days to find a match. If a match cannot be made within seven days, the claim will be processed without the attachment and will be denied if an attachment is required. When such a claim is denied, both the paper attachment(s) and the electronic claim will need to be resubmitted.
Providers are required to send paper attachments relating to electronic claim transactions to the following address:
ForwardHealth
Claims and Adjustments
313 Blettner Blvd
Madison WI 53784
This does not apply to compound and noncompound claims. Topic #11677 Uploading Claim Attachments Via the Portal
Providers are able to upload attachments for most claims via the secure Provider area of the ForwardHealth Portal. This allows providers to submit all components for claims electronically.
Providers are able to upload attachments via the Portal when a claim is suspended and an attachment was indicated but not yet received. Providers are able to upload attachments for any suspended claim that was submitted electronically. Providers should note that all attachments for a suspended claim must be submitted within the same business day.
Claim Types
Providers will be able to upload attachments to claims via the Portal for the following claim types:
- Professional
- Institutional
- Dental
The submission policy for compound and noncompound drug claims does not allow attachments.
Document Formats
Providers are able to upload documents in the following formats:
- JPEG (.jpg or .jpeg)
- PDF (.pdf)
- Rich Text Format (.rtf)
- Text File (.txt)
JPEG files must be stored with a .jpg or .jpeg extension; text files must be stored with a .txt extension; rich text format files must be stored with a .rtf extension; and PDF files must be stored with a .pdf extension.
Microsoft Word files (.doc) cannot be uploaded but can be saved and uploaded in Rich Text Format or Text File formats.
Uploading Claim Attachments
Claims Submitted by Direct Data Entry
When a provider submits a DDE claim and indicates an attachment will also be included, a feature button will appear and link to the DDE claim screen where attachments can be uploaded.
Providers are still required to indicate on the DDE claim that the claim will include an attachment via the Attachments panel.
Claims will suspend for seven days before denying for not receiving the attachment.
Claims Submitted by Provider Electronic Software and 837 Health Care Claim Transactions
Providers submitting claims via 837 transactions are required to indicate attachments via the PWK segment. Providers submitting claims via PES software will be required to indicate attachments via the attachment control field. Once the claim has been submitted, providers will be able to search for the claim on the Portal and upload the attachment via the Portal. Refer to the Implementation Guides for how to use the PWK segment in 837 transactions and the PES Manual for how to use the attachment control field.
Claims will suspend for seven days before denying for not receiving the attachment. Topic #3385 Vehicle Without Wheelchair Ramp or Lift
When billing for services provided in an HSV that is not equipped with a wheelchair ramp or lift, providers are required to use the following procedure codes:
- A0120 (Non-emergency transportation: mini-bus, mountain area transports, or other transportation systems)
- S0215 (Non-emergency transportation: mileage, per mile)
|