| Program Name: | BadgerCare Plus and Medicaid | Handbook Area: | Physician | | 05/04/2024 | Claims : ResponsesTopic #540 An Overview of the Remittance Advice
The RA provides important information about the processing of claims and adjustment requests as well as additional financial transactions such as refunds or recoupment amounts withheld. ForwardHealth provides electronic RAs to providers on their secure ForwardHealth Portal accounts when at least one claim, adjustment request, or financial transaction is processed. RAs are generated from the appropriate ForwardHealth program when at least one claim, adjustment request, or financial transaction is processed. An RA is generated regardless of how a claim or adjustment is submitted (electronically or on paper). Generally, payment information is released and an RA is generated by ForwardHealth no sooner than the first state business day following the financial cycle.
Providers are required to access their secure ForwardHealth provider Portal account to obtain their RA.
RAs are accessible to providers in a TXT format via the secure Provider area of the Portal. Providers are also able to download the RA from their secure provider Portal account in a CSV format. Topic #5091 National Provider Identifier on the Remittance Advice
Health care providers who have a single NPI that is used for multiple enrollments will receive an RA for each enrollment with the same NPI reported on each of the RAs. For instance, if a hospital has obtained a single NPI and the hospital has a clinic, a lab, and a pharmacy that are all enrolled in Wisconsin Medicaid, the clinic, the lab, and the pharmacy will submit separate claims that indicate the same NPI as the hospital. Separate RAs will be generated for the hospital, the clinic, the lab, and the pharmacy. Topic #4818 Calculating Totals on the Remittance Advice for Adjusted and Paid Claims
The total amounts for all adjusted or paid claims reported on the RA appear at the end of the adjusted claims and paid claims sections. ForwardHealth calculates the total for each section by adding the net amounts for all claims listed in that section. Cutback amounts are subtracted from the allowed amount to reach the total reimbursement for the claims.
Note: Some cutbacks that are reported in detail lines will appear as EOB codes and will not display an exact dollar amount. Topic #534 Claim Number
Each claim or adjustment request received by ForwardHealth is assigned a unique claim number (also known as the ICN). However, denied real-time compound and noncompound claims are not assigned an ICN, but receive an authorization number. Authorization numbers are not reported to the RA or 835.
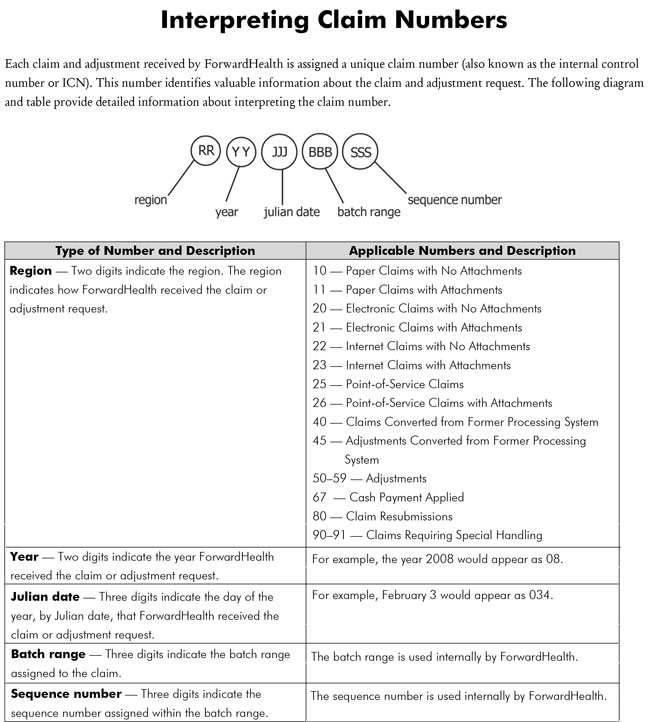
Interpreting Claim Numbers
The ICN consists of 13 digits that identify valuable information (e.g., the date the claim was received by ForwardHealth, how the claim was submitted) about the claim or adjustment request.
 Topic #535 Claim Status
ForwardHealth generally processes claims and adjustment requests within 30 days of receipt. Providers may check the status of a claim or adjustment request using the AVR system or the 276/277 transaction.
If a claim or adjustment request does not appear in claim status within 45 days of the date of submission, a copy of the original claim or adjustment request should be resubmitted through normal processing channels. Topic #22277 Claims Denial Adjustment/Review Request
Providers should take the following steps if they are uncertain about why particular services on a claim were denied:
- Review ForwardHealth remittance information for the specific reason for the denial.
- Review the claim submitted to ensure all information is accurate and complete.
- Consult recent CPT and HCPCS publications to make sure proper coding instructions were followed.
- Consult recent ForwardHealth publications to make sure current policy and billing instructions were followed.
- Call Provider Services for further information or explanation.
- Review the ForwardHealth Adjustment/Reconsideration Request process and submit a request if appropriate.
If a provider disagrees with a claim determination, the provider may take one of two actions.
- If the claim is denied, the provider may resubmit the claim with supporting documentation to Provider Services Written Correspondence using the Written Correspondence form with the "other (briefly explain the situation in question below)" box checked and the words "medical consultant review requested" written on the form.
- If the original claim is in an allowed status, the provider may submit an Adjustment/Reconsideration Request form with supporting documentation and the "medical consultant review requested" box checked on the form to Provider Services Written Correspondence.
Topic #644 Information is available for DOS before February 12, 2022.
ClaimsXten Review
ForwardHealth monitors all professional claims for compliance with reimbursement policy using an automated procedure coding review software known as Change Healthcare ClaimsXten. ClaimsXten reviews claims submitted for billing inconsistencies and errors during claims processing. Medicaid programs in other states, insurance companies, and Medicare all use similar software.
EOB codes specific to the ClaimsXten review appear in the TXT RA file and in the electronic 835 transactions.
ClaimsXten review does not change Medicaid or BadgerCare Plus policy on covered services but monitors compliance with policy more closely and reimburses providers appropriately.
ClaimsXten will be reviewed on a regular basis and changes will be made as needed based on industry best practices. In addition to adding new procedure codes, ClaimsXten may add or revise claim editing information based on an ongoing review of the software knowledge base. This ongoing process helps to ensure that the default clinical content used in ClaimsXten is clinically appropriate and within national standards.
Areas Monitored by ClaimsXten
ClaimsXten uses rules to monitor certain claim situations.
ClaimsXten rules adopted by ForwardHealth are subject to change or revision. This is not a comprehensive list of all claim edits, but rather examples of areas where edit rules will be implemented via ClaimsXten. Reference to more specific ForwardHealth coverage and reimbursement policy, where applicable, is indicated.
ForwardHealth uses ClaimsXten software to monitor the following situations:
- Unbundled and rebundled procedures
- Incidental/integral procedures
- Mutually exclusive procedures
- Medical visit billing errors
- Preoperative and postoperative billing errors
- Assistant surgeon billing errors
ClaimsXten will not review claims that have been denied for general billing errors, such as an invalid member identification number or an invalid or missing provider number. Providers will need to correct the general billing error and resubmit the claim, at which point ClaimsXten will review the claim.
Unbundled and Rebundled Procedures
Unbundling occurs when two or more procedure codes are used to describe a procedure that may be better described by a single, more comprehensive procedure code. ClaimsXten considers the single, most appropriate procedure code for reimbursement when unbundling is detected.
If certain procedure codes are submitted, ClaimsXten rebundles them into the single most appropriate procedure code. For example, if a provider submits a claim with two or more procedure codes for the same type of wound with varying sizes, ClaimsXten rebundles them to a procedure code that would encompass the total size.
ClaimsXten will also total billed amounts for individual procedures. For example, if the provider bills three procedures at $20, $30, and $25, ClaimsXten rebundles them into a single procedure code, adds the three amounts, and calculates the billed amount for a new rebundled code at $75. Then, ForwardHealth reimburses the provider either the lesser of the billed amounts or the maximum allowable fee for that rebundled procedure code.
Incidental/Integral Procedures
Incidental procedures are those procedures performed at the same time as a more complex primary procedure. These require few additional provider resources and are generally not considered necessary to the performance of the primary procedure. For example, the removal of an asymptomatic appendix is considered an incidental procedure when done during hysterectomy surgery.
Integral procedures are those procedures performed as part of a more complex primary procedure. For example, when a member undergoes a transurethral incision of the prostate, the scope procedure is considered integral to the performance of the prostate procedure and would be denied as a separately billed item.
When a procedure is either incidental or integral to a major procedure, ClaimsXten considers only the primary procedure for reimbursement.
Mutually Exclusive Procedures
Mutually exclusive procedures are procedures that would not be performed on a single member on the same day or that use different codes to describe the same type of procedure.
An example of a mutually exclusive situation is when the repair of the organ can be performed by two different methods. One repair method must be chosen to repair the organ and must be reported. A second example is the reporting of an "initial" service and a "subsequent" service. It is contradictory for a service to be classified as both an initial and a subsequent service at the same time.
When two or more procedures are mutually exclusive, ForwardHealth considers for reimbursement the procedure code with the highest provider-billed amount and denies the other code.
Medical Visit Billing Errors
Medical visit billing errors occur if E&M services are reported separately when a substantial diagnostic or therapeutic procedure is performed. Under CMS guidelines, most E&M procedures are not allowed to be reported separately when a substantial diagnostic or therapeutic procedure is performed.
ClaimsXten monitors medical visits based on the type of E&M service (that is, initial or new patient; or follow-up or established patient services) and the complexity (that is, major or minor) of the accompanying procedure.
For example, if a provider submits a procedure code for a major surgical procedure as well as for the initial hospital care per day, ClaimsXten denies the initial hospital care procedure as a visit when submitted with the major procedure with the same date of service. The major procedure has a 90-day global surgical period and the postoperative visit is not separately reimbursable.
Preoperative and Postoperative Billing Errors
Preoperative and postoperative billing errors occur when E&M services are billed with surgical procedures during their preoperative and postoperative periods. ClaimsXten bases the preoperative and postoperative periods on designations in the CMS National Physician Fee Schedule.
For example, if a provider submits a procedure code for an office visit for E&M with a DOS of 11/02/21 and a related surgical procedure with a DOS of 11/03/21, ClaimsXten may deny the procedure code for the office visit as a preoperative visit.
Assistant Surgeon Billing Errors
ClaimsXten develops and maintains assistant surgeon values using the CMS Physician Fee Schedule as its primary source. Providers should refer to the Medicare Physician Fee Schedule for procedure codes where a surgery assistant may be paid. These codes are denoted with an indicator of "2" in the Assistant at Surgery column of the Medicare Physician Fee Schedule.
ForwardHealth's Assistant Surgeon Fee Schedule reflects procedure codes allowable with an assistant surgeon designation consistent with ClaimsXten.
For example, if a provider bills a procedure code for a surgery with a modifier representing an assistant surgeon, and ClaimsXten determines that the procedure does not require an assistant surgeon, the procedure-modifier combination will be denied. Topic #4746 Cutback Fields on the Remittance Advice for Adjusted and Paid Claims
Cutback fields indicate amounts that reduce the allowed amount of the claim. Examples of cutbacks include other insurance, member copayment, spenddown amounts, deductibles, or patient liability amounts. Amounts indicated in a cutback field are subtracted from the total allowed reimbursement.
Providers should note that cutback amounts indicated in the header of an adjusted or paid claim section apply only to the header. Not all cutback fields that apply to a detail line (such as copayments or spenddowns) will be indicated on the RA; the detail line EOB codes inform providers that an amount was deducted from the total reimbursement but may not indicate the exact amount.
Note: Providers who receive 835 transactions will be able to see all deducted amounts on paid and adjusted claims. Topic #8617 Duplicate Claim Denials Within Seven Days
If a pharmacy's drug claim with an NDC is received by ForwardHealth and a subsequent professional claim for the same drug is received from a clinic with the equivalent drug-related HCPCS procedure code having a DOS that is within seven days of the pharmacy's DOS, then the clinic's claim will be denied as a duplicate claim. For example, a member may receive albuterol inhalation solution at a clinic and then fill a prescription at the pharmacy for the same drug within seven days. If the first claim received is the pharmacy's drug claim, it will be paid if all billing requirements are met.
These denied claims should be submitted on paper to the following address:
ForwardHealth
Provider Services Written Correspondence
313 Blettner Blvd
Madison WI 53784 Topic #537 Electronic Remittance Information
Providers are required to access their secure ForwardHealth provider Portal account to obtain their RAs. Electronic RAs on the Portal are not available to the following providers because these providers are not allowed to establish Portal accounts by their Provider Agreements:
- In-state emergency providers
- Out-of-state providers
- Out-of-country providers
RAs are accessible to providers in a TXT format or from a CSV file via the secure Provider area of the Portal.
Text File
The TXT format file is generated by financial payer and listed by RA number and RA date on the secure provider Portal account under the "View Remittance Advices" menu. RAs from the last 121 days are available in the TXT format. When a user clicks on an RA, a pop-up window displays asking if the user would like to "Open" or "Save" the file. If "Open" is chosen, the document opens based on the user's application associated with opening text documents. If "Save" is chosen, the "Save As" window will open. The user can then browse to a location on their computer or network to save the document.
Users should be aware that "Word Wrap" must be turned off in the Notepad application. If it is not, it will cause distorted formatting. Also, users may need to resize the Notepad window to view all of the data. Providers wanting to print their files must ensure that the "Page Setup" application is set to the "Landscape" setting; otherwise, the printed document will not contain all the information.
Comma-Separated Values Downloadable File
A CSV file is a file format accepted by a wide range of computer software programs. Downloadable CSV-formatted RAs allow users the benefits of building a customized RA specific to their use and saving the file to their computer. The CSV file on a provider's Portal appears as linear text separated by commas until it is downloaded into a compatible software program. Once downloaded, the file may be saved to a user's computer and the data manipulated, as desired.
To access the CSV file, providers should select the "View Remittance Advices" menu at the top of the provider's Portal home page.
The CSV files are generated per financial payer and listed by RA number and RA date. A separate CSV file is listed for the last 10 RAs. Providers can select specific sections of the RA by date to download, making the information easy to read and organize.
The CSV file may be downloaded into a Microsoft Office Excel spreadsheet or into another compatible software program, such as Microsoft Office Access or OpenOffice. OpenOffice is a free software program obtainable from the internet. Google Docs and ZDNet also offer free spreadsheet applications. Microsoft Office Excel, a widely used program, is a spreadsheet application for Microsoft Windows and Mac OS. The 1995 Office Excel for Windows (Version 7.0) included in Office 95 or a newer version is recommended for maximum file capabilities when downloading the CSV file. Earlier versions of Microsoft Office Excel will work with the CSV file; however, files exceeding 65,000 lines may need to be split into smaller files when downloading using earlier versions. Microsoft Office Access can manage larger data files.
Refer to the CSV User Guide on the User Guides page of the Portal for instructions about Microsoft Office Excel functions that can be used to manipulate RA data downloaded from the CSV file.
835
Electronic remittance information may be obtained using the 835 transaction. It provides useful information regarding the processing of claims and adjustment requests, which includes the status or action taken on a claim; claim detail, adjustment, or adjustment detail for all claims and adjustments processed that week, regardless of whether they are reimbursed or denied. However, a real-time compound or noncompound claim will not appear on remittance information if the claim is denied by ForwardHealth. ForwardHealth releases payment information to the 835 no sooner than on the first state business day following the financial cycle.
Provider Electronic Solutions Software
ForwardHealth offers electronic billing software at no cost to providers. The PES software allows providers to submit electronic claims and claim reversals and to download the 835 transaction. To obtain PES software, providers may download it from the ForwardHealth Portal. For assistance installing and using PES software, providers may call the EDI Helpdesk. Topic #4822 Explanation of Benefit Codes in the Claim Header and in the Detail Lines
EOB codes are four-digit numeric codes specific to ForwardHealth that correspond to a printed message about the status or action taken on a claim, claim detail, adjustment, or adjustment detail.
The claim processing sections of the RA report EOBs for the claim header information and detail lines, as appropriate. Header information is a summary of the information from the claim, such as the DOS that the claim covers or the total amount paid for the claim. Detail lines report information from the claim details, such as specific procedure codes or revenue codes, the amount billed for each code, and the amount paid for a detail line item.
Header EOBs are listed below the claim header information and pertain only to the header information. Detail line EOBs are listed after each detail line and pertain only to the detail line.
TEXT File
EOB codes and descriptions are listed in the RA information in the TXT file.
CSV File
EOB codes are listed in the RA information from the CSV file; however, the printed messages corresponding to the codes do not appear in the file. The EOB Code Listing matching standard EOB codes to explanation text is available on the Portal for reference. Topic #13437 ForwardHealth-Initiated Claim Adjustments
There are times when ForwardHealth must initiate a claim adjustment to address claim issues that do not require provider action and do not affect reimbursement.
Claims that are subject to this type of ForwardHealth-initiated claim adjustment will have EOB code 8234 noted on the RA.
The adjusted claim will be assigned a new claim number, known as an ICN. The new ICN will begin with "58." If the provider adjusts this claim in the future, the new ICN will be required when resubmitting the claim. Topic #4820 Identifying the Claims Reported on the Remittance Advice
The RA reports the first 12 characters of the MRN and/or a PCN, also referred to as Patient Account Number, submitted on the original claims. The MRN and PCN fields are located beneath the member's name on any section of the RA that reports claims processing information.
Providers are strongly encouraged to enter these numbers on claims. Entering the MRN and/or the PCN on claims may assist providers in identifying the claims reported on the RA.
Note: Claims processing sections for dental and drug claims do not include the MRN or the PCN. Topic #11537 National Correct Coding Initiative
As part of the federal PPACA of 2010, the federal CMS are required to promote correct coding and control improper coding leading to inappropriate payment of claims under Medicaid. The NCCI is the CMS response to this requirement. The NCCI includes the creation and implementation of claims processing edits to ensure correct coding on claims submitted for Medicaid reimbursement.
ForwardHealth is required to implement the NCCI in order to monitor all professional claims and outpatient hospital claims submitted with CPT or HCPCS procedure codes for Wisconsin Medicaid, BadgerCare Plus, WCDP, and Family Planning Only Services for compliance with the following NCCI edits:
- MUE, or units-of-service detail edits
- Procedure-to-procedure detail edits
The NCCI editing will occur in addition to/along with current procedure code review and editing completed by Change Healthcare ClaimsXten and in ForwardHealth interChange.
Medically Unlikely Detail Edits
MUE, or units-of-service detail edits, define the maximum units of service that a provider would report under most circumstances for a single member on a single DOS for each CPT or HCPCS procedure code. If a detail on a claim is denied for MUE, providers will receive an EOB code on the RA indicating that the detail was denied due to NCCI.
An example of an MUE would be if procedure code 11102 (tangential biopsy of skin [eg, shave, scoop, saucerize, curette]; single lesion) was billed by a provider on a professional claim with a quantity of two or more. This procedure is medically unlikely to occur more than once; therefore, if it is billed with units greater than one, the detail will be denied.
Procedure-to-Procedure Detail Edits
Procedure-to-procedure detail edits define pairs of CPT or HCPCS codes that should not be reported together on the same DOS for a variety of reasons. This edit applies across details on a single claim or across different claims. For example, an earlier claim that was paid may be denied and recouped if a more complete code is billed for the same DOS on a separate claim. If a detail on a claim is denied for procedure-to-procedure edit, providers will receive an EOB code on the RA indicating that the detail was denied due to NCCI.
An example of a procedure-to-procedure edit would be if procedure codes 11451 (excision of skin and subcutaneous tissue for hidradenitis, axillary; with complex repair) and 93000 (electrocardiogram, routine ECG with at least 12 leads; with interpretation and report) were billed on the same claim for the same DOS. Procedure code 11451 describes a more complex service than procedure code 93000, and therefore, the secondary procedure would be denied.
Quarterly Code List Updates
CMS will issue quarterly revisions to the table of codes subject to NCCI edits that ForwardHealth will adopt and implement. Refer to the CMS Medicaid website for downloadable code lists.
Claim Details Denied as a Result of National Correct Coding Initiative Edits
Providers should take the following steps if they are uncertain why particular services on a claim were denied:
- Review ForwardHealth remittance information for the EOB message related to the denial.
- Review the claim submitted to ensure all information is accurate and complete.
- Consult current CPT and HCPCS publications to make sure proper coding instructions were followed.
- Consult current ForwardHealth publications, including the Online Handbook, to make sure current policy and billing instructions were followed.
- Call Provider Services for further information or explanation.
If reimbursement for a claim or a detail on a claim is denied due to an MUE or procedure-to-procedure edit, providers may appeal the denial. Following are instructions for submitting an appeal:
- Complete the Adjustment/Reconsideration Request form. In Element 16, select the "Consultant review requested" checkbox and the "Other/comments" checkbox. In the "Other/comments" text box, indicate "Reconsideration of an NCCI denial."
- Attach notes/supporting documentation.
- Submit a claim, Adjustment/Reconsideration Request, and additional notes/supporting documentation to ForwardHealth for processing.
Topic #539 Obtaining the Remittance Advice
Providers are required to access their secure ForwardHealth provider Portal account to obtain RAs. The secure Portal allows providers to conduct business and exchange electronic transactions with ForwardHealth. A separate Portal account is required for each financial payer.
Providers who do not have a ForwardHealth provider Portal account may request one.
RAs are accessible to providers in a TXT format via the secure provider Portal account. The TXT format file is generated per financial payer and listed by RA number and RA date on the secure provider Portal account under "View Remittance Advices" menu at the top of the provider's Portal home page. RAs from the last 121 days are available in the TXT format.
Providers can also access RAs in a CSV format from their secure provider Portal account. The CSV files are generated per financial payer and listed by RA number and RA date on the secure provider Portal account under "View Remittance Advices" menu at the top of the provider's Portal home page. A separate CSV file is listed for the last 10 RAs. Topic #4745 Overview of Claims Processing Information on the Remittance Advice
The claims processing sections of the RA include information submitted on claims and the status of the claims. The claim status designations are paid, adjusted, or denied. The RA also supplies information about why the claim was adjusted or denied or how the reimbursement was calculated for the payment.
The claims processing information in the RA is grouped by the type of claim and the status of the claim. Providers receive claims processing sections that correspond to the types of claims that have been finalized during the current financial cycle.
The claims processing sections reflect the types of claims submitted, such as the following:
- Compound drug claims
- Dental claims
- Noncompound drug claims
- Inpatient claims
- Long term care claims
- Medicare crossover institutional claims
- Medicare crossover professional claims
- Outpatient claims
- Professional claims
The claims processing sections are divided into the following status designations:
- Adjusted claims
- Denied claims
- Paid claims
| Claim Types |
Provider Types |
| Dental claims |
Dentists, dental hygienists, HealthCheck agencies that provide dental services |
| Inpatient claims |
Inpatient hospital providers and institutes for mental disease providers |
| Long term care claims |
Nursing homes |
| Medicare crossover institutional claims |
Most providers who submit claims on the UB-04 |
| Medicare crossover professional claims |
Most providers who submit claims on the 1500 Health Insurance Claim Form |
| Noncompound and compound drug claims |
Pharmacies and dispensing physicians |
| Outpatient claims |
Outpatient hospital providers and hospice providers |
| Professional claims |
Ambulance providers, ambulatory surgery centers, anesthesiologist assistants, audiologists, case management providers, certified registered nurse anesthetists, chiropractors, community care organizations, community support programs, crisis intervention providers, day treatment providers, family planning clinics, federally qualified health centers, HealthCheck providers, HealthCheck "Other Services" providers, hearing instrument specialists, home health agencies, independent labs, individual medical supply providers, medical equipment vendors, mental health/substance abuse clinics, nurses in independent practice, nurse practitioners, occupational therapists, opticians, optometrists, personal care agencies, physical therapists, physician assistants, physician clinics, physicians, podiatrists, portable X-ray providers, prenatal care coordination providers, psychologists, rehabilitation agencies, respiratory therapists, rural health clinics, school-based services providers, specialized medical vehicle providers, speech and hearing clinics, speech-language pathologists, therapy groups |
Topic #4821 Prior Authorization Number on the Remittance Advice
The RA reports PA numbers used to process the claim. PA numbers appear in the detail lines of claims processing information. Topic #4418 Reading Non-Claims Processing Sections of the Remittance Advice
Address Page
In the TXT file, the Address page displays the provider name and "Pay to" address of the provider.
Banner Messages
The Banner Messages section of the RA contains important, time-sensitive messages for providers. For example, banner messages might inform providers of claim adjustments initiated by ForwardHealth, claim submission deadlines, and dates of upcoming training sessions. It is possible for each RA to include different messages; therefore, providers who receive multiple RAs should read all of their banner messages.
Banner messages appear on the TXT file but not on the CSV file. Banner messages are posted in the "View Remittance Advices" menu on the provider's secure Portal account.
Explanation of Benefits Code Descriptions
EOB code descriptions are listed in the RA information in the TXT file.
EOB codes are listed in the RA information from the CSV file; however, the printed messages corresponding to the codes do not appear in the file.
Financial Transactions Page
The Financial Transactions section details the provider's weekly financial activity. Financial transactions reported on the RA include payouts, refunds, accounts receivable, and payments for claims.
Payouts are payments made to the provider by ForwardHealth that do not correspond to a specific claim (that is, nursing home assessment reimbursement).
Refunds are payments made to providers for overpayments.
The Accounts Receivable section displays the accounts receivable for amounts owed by providers. The accounts receivable is set to automatically recover any outstanding balance so that money owed is automatically recouped from the provider. If the full amount cannot be recouped during the current financial cycle, an outstanding balance will appear in the "Balance" column.
In the Accounts Receivable section, the "Amount Recouped In Current Cycle" column, when applicable, shows the recoupment amount for the financial cycle as a separate number from the "Recoupment Amount To Date." The "Recoupment Amount To Date" column shows the total amount recouped for each accounts receivable, including the amount recouped in the current cycle. The "Total Recoupment" line shows the sum of all recoupments to date in the "Recoupment Amount To Date" column and the sum of all recoupments for the current financial cycle in the "Amount Recouped In Current Cycle" column.
For decreasing claim adjustments listed on the RA, a separate accounts receivable will be established and will be listed in the Financial Transactions section. The accounts receivable will be established for the entire amount of the original paid claim. Providers will see net difference between the claim and the adjustment reflected on the RA.
Each new claim adjustment is assigned an identification number called the "Adjustment ICN." For other financial transactions, the adjustment ICN is determined by the following formula.
| Type of Character and Description |
Applicable Characters and Description |
| Transaction—The first character indicates the type of financial transaction that created the accounts receivable. |
V—Capitation adjustment
1—OBRA Level 1 screening void request
2—OBRA Nurse Aide Training/Testing void request |
| Identifier—10 additional numbers are assigned to complete the Adjustment ICN. |
The identifier is used internally by ForwardHealth. |
Service Code Descriptions
The Service Code Descriptions section lists all the service codes (that is, procedure codes or revenue codes) reported on the RA with their corresponding descriptions.
Summary
The Summary section reviews the provider's claim activity and financial transactions with the payer (Medicaid, ADAP, WCDP, or WWWP) for the current financial cycle, the month-to-date, and the year-to-date, if applicable.
Under the "Claims Data" heading, providers can review the total number of claims that have been paid, adjusted, or denied along with the total amount reimbursed for all paid and adjusted claims. Only WWWP providers will see amounts reported for "Claims in Process." Other providers will always see zeroes in these fields.
Under the "Earnings Data" heading, providers will see total reimbursement amounts for other financial transactions, such as reimbursement for OBRA Level 1 screening, reimbursement for OBRA Nurse Aid Training/Testing, and capitation payments.
Note: HMOs should note that capitation payments are only reported in the Summary section of the RA. HMOs receive supplemental reports of their financial transactions from ForwardHealth.
The "Earnings Data" portion also summarizes refunds and voids and reports the net payment for the current financial cycle, the month-to-date, and the year-to-date, if applicable.
Providers should note that the Summary section will include outstanding checks 90 days after issuance and/or payments made to lien holders, if applicable. Topic #368 Reading the Claim Adjustments Section of the Remittance Advice
Providers receive a Claim Adjustments section in the RA if any of their claims were adjusted during the current financial cycle. A claim may be adjusted because one of the following occurred:
- An adjustment request was submitted by the provider.
- ForwardHealth initiated an adjustment.
- A cash refund was submitted to ForwardHealth.
To adjust a claim, ForwardHealth recoups the difference—or pays the difference—between the original claim amount and the claim adjustment amount. This difference will be reflected on the RA.
In the Claim Adjustments section, the original claim information in the claim header is surrounded by parentheses. Information about the claim adjustment appears directly below the original claim header information. Providers should check the Adjustment EOB code(s) for a summary of why the claim was adjusted; other header EOBs will provide additional information.
The Claim Adjustments section only lists detail lines for a claim adjustment if that claim adjustment has detail line EOBs. This section does not list detail lines for the original paid claim.
Note: For adjusted compound and noncompound claims, only the compound drug sections include detail lines.
Below the claim header and the detail information will be located one of three possible responses with a corresponding dollar amount: "Additional Payment," "Overpayment To Be Withheld," or "Refund Amount Applied." The response indicated depends on the difference between the original claim amount and the claim adjustment amount.
If the difference is a positive dollar amount, indicating that ForwardHealth owes additional monies to the provider, then the amount appears in the "Additional Payment" line.
If the difference is a negative dollar amount, indicating that the provider owes ForwardHealth additional monies, then the amount appears in the "Overpayment To Be Withheld" line. ForwardHealth automatically withholds this amount from payments made to the provider during the same financial cycle or during subsequent financial cycles, if necessary. This amount also appears in the Financial Transactions section as an outstanding balance under "Accounts Receivable."
An amount appears for "Refund Amount Applied" if ForwardHealth makes a payment to refund a cash receipt to a provider. Topic #4824 Reading the Claims Denied Section of the Remittance Advice
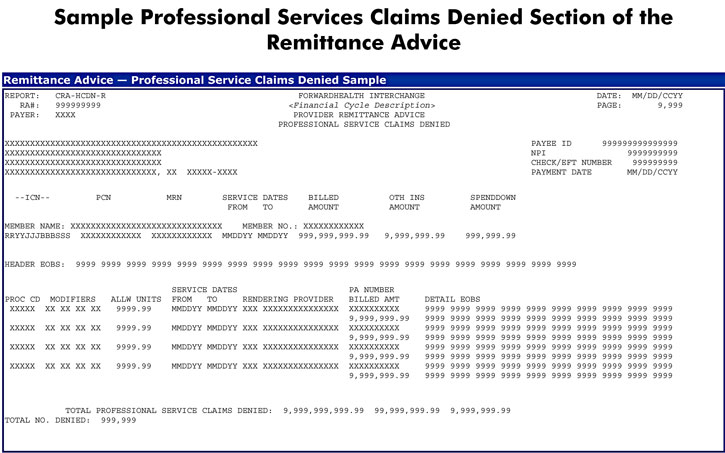
Providers receive a Claims Denied section in the RA if any of their claims were denied during the current financial cycle.
In the denied claims section, providers will see the original claim header information reported along with EOB codes for the claim header and the detail lines, as applicable. Providers should refer to the EOB Code Description section of the RA to determine why the claim was denied.
 Topic #4825 Reading the Claims Paid Section of the Remittance Advice
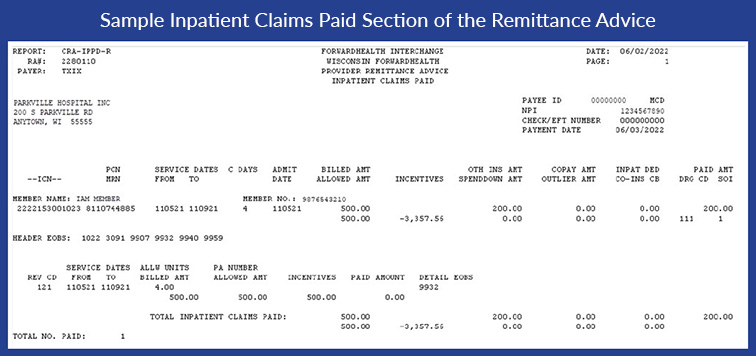
Providers receive a Claims Paid section in the RA if any of their claims were determined payable during the current financial cycle.
In a paid claims section, providers will see the original claim information reported along with EOB codes for both the header and the detail lines, if applicable. Providers should refer to the EOB Code Description section of the RA for more information about how the reimbursement amount was determined. The Incentives column is calculated in accordance with the 835 standards to balance between the service line, the claim, and the transaction.
 Topic #4828 Remittance Advice Financial Cycles
Each financial payer (Medicaid, ADAP, WCDP, and WWWP) has separate financial cycles that occur on different days of the week. RAs are generated and posted to secure provider Portal accounts after each financial cycle is completed. Therefore, RAs may be generated and posted to secure provider ForwardHealth Portal accounts from different payers on different days of the week.
Certain financial transactions may run on a daily basis, including non-claim related payouts and stop payment reissues. Providers may have access to the RAs generated and posted to secure provider Portal accounts for these financial transactions at any time during the week. Topic #4827 Remittance Advice Generated by Payer and by Provider Enrollment
RAs are generated and posted to secure provider Portal accounts from one or more of the following ForwardHealth financial payers:
- Wisconsin Medicaid (Wisconsin Medicaid is the financial payer for the Medicaid, BadgerCare Plus, and SeniorCare programs)
- ADAP
- WCDP
- WWWP
A separate Portal account is required for each financial payer.
Note: Each of the four payers generate separate RAs for the claims, adjustment requests, or other financial transactions submitted to the payer. A provider who submits claims, adjustment requests, or other financial transactions to more than one of these payers may receive several RAs.
The RA is generated per provider enrollment. Providers who have a single NPI that is used for multiple enrollments should be aware that an RA will be generated for each enrollment, but the same NPI will be reported on each of the RAs.
For instance, a hospital has obtained a single NPI. The hospital has a clinic, a lab, and a pharmacy that are all enrolled with ForwardHealth. The clinic, the lab, and the pharmacy submit separate claims that indicate the same NPI as the hospital. Separate RAs will be generated for the hospital, the clinic, the lab, and the pharmacy. Topic #6237 Reporting a Lost Check
To report a lost check to ForwardHealth, providers are required to mail or fax a letter to ForwardHealth Financial Services. Providers are required to include the following information in the letter:
- Provider's name and address, including the ZIP+4 code
- Provider's identification number
- For healthcare providers, include the NPI and taxonomy code.
- For non-healthcare providers, include the provider identification number.
- Check number, check date, and check amount (This should be recorded on the RA.)
- A written request to stop payment and reissue the check
- The signature of an authorized financial representative (An individual provider is considered his or her own authorized financial representative.)
Fax the letter to ForwardHealth at 608-221-4567 or mail it to the following address:
ForwardHealth
Financial Services
313 Blettner Blvd
Madison WI 53784 Topic #5018 Searching for and Viewing All Claims on the Portal
All claims, including compound, noncompound, and dental claims, are available for viewing on the ForwardHealth Portal.
To search and view claims on the Portal, providers may do the following:
- Go to the Portal.
- Log in to the secure Provider area of the Portal.
- The most recent claims processed by ForwardHealth will be viewable on the provider's home page or the provider may select "claim search" and enter the applicable information to search for additional claims.
- Select the claim the provider wants to view.
Topic #4829 Sections of the Remittance Advice
The RA information in the TXT file includes the following sections:
- Address page
- Banner messages
- Paper check information, if applicable
- Claims processing information
- EOB code descriptions
- Financial transactions
- Service code descriptions
- Summary
- Claim sequence numbers
The RA information in the CSV file includes the following sections:
- Payment
- Payment hold
- Service codes and descriptions
- Financial transactions
- Summary
- Inpatient claims
- Outpatient claims
- Professional claims
- Medicare crossovers—Professional
- Medicare crossovers—Institutional
- Compound drug claims
- Noncompound drug claims
- Dental claims
- Long term care claims
- Financial transactions
- Summary
- Claim sequence numbers
Providers can select specific sections of the RA in the CSV file within each RA date to be downloaded making the information easy to read and to organize.
Remittance Advice Header Information
The first page of each section of the RA (except the address page of the TXT file) displays the same RA header information.
The following fields are on the left-hand side of the header:
- The technical name of the RA section (for example, CRA-TRAN-R), which is an internal ForwardHealth designation
- The RA number, which is a unique number assigned to each RA that is generated
- The name of the payer (Medicaid, ADAP, WCDP, or WWWP)
- The "Pay to" address of the provider. The "Pay to" address is used for mailing purposes.
The following information is in the middle of the header:
- A description of the financial cycle
- The name of the RA section (for example, "Financial Transactions" or "Professional Services Claims Paid")
The right-hand side of the header reports the following information:
- The date of the financial cycle and date the RA was generated
- The page number
- The "Payee ID" of the provider. A payee ID is defined as the identification number of a unique entity receiving payment for goods and/or services from ForwardHealth. The payee ID is up to 15 characters long and may be based on a pre-existing identification number, such as the Medicaid provider number. The payee ID is an internal ForwardHealth designation. The Medicaid provider number will display in this field for providers who do not have an NPI.
- The NPI of the provider, if applicable. This field will be blank for those providers who do not have an NPI.
- The number of the check issued for the RA, if applicable
- The date of payment on the check, if applicable
Topic #544 Verifying Accuracy of Claims Processing
After obtaining ForwardHealth remittance information, providers should compare it to the claims or adjustment requests to verify that ForwardHealth processed elements of the claims or adjustment requests as submitted. To ensure correct reimbursement, providers should do the following:
- Identify and correct any discrepancy that affected the way a claim processed.
- Correct and resubmit claims that are denied.
- Submit an adjustment request for allowed claims that require a change or correction.
When posting a payment or denial to a member's account, providers should note the date on the ForwardHealth remittance information that indicates that the claim or adjustment has finalized. Providers are required to supply this information if further follow-up actions are necessary. |