| Program Name: | BadgerCare Plus and Medicaid | Handbook Area: | Pharmacy | | 05/07/2024 | Prior Authorization : Submission OptionsTopic #12597 278 Health Care Services Review — Request for Review and Response Transaction
Providers may request PA electronically using the 278 transaction, the standard electronic format for health care service PA requests.
Compliance Testing
Trading partners may conduct compliance testing for the 278 transaction.
After receiving an "accepted" 999 for a test 278 transaction, trading partners are required to call the EDI Helpdesk to request the production 278 transaction set be assigned to them.
Submitting Prior Authorization Requests
Submitting an initial PA request using the 278 transaction does not result in a real-time approval and cannot be used to request PA for drugs and diabetic supplies.
After submitting a PA request via a 278 transaction, providers will receive a real-time response indicating whether the transaction is valid or invalid. If the transaction is invalid, the response will indicate the reject reason(s), and providers can correct and submit a new PA request using the 278 transaction. A real-time response indicating a valid 278 transaction will include a PA number and a pending status. The PA request will be placed in a status of "Pending - Fiscal Agent Review."
The 278 transaction does not allow providers to submit supporting clinical information as required to adjudicate the PA request.
Trading partners cannot submit the 278 transaction through PES. In order to submit the 278 transaction, trading partners will need to use their own software or contract with a software vendor. Topic #7857 Drug Authorization and Policy Override Center
The DAPO Center is a specialized drug help desk for prescribers, their designees, and pharmacy providers to submit PA requests for anti-obesity drugs and to request policy overrides for other drugs or diabetic supplies over the phone. After business hours, providers may leave a voicemail message for DAPO Center staff to return the next business day.
The DAPO Center is staffed by certified pharmacy technicians.
Prior Authorization Requests and Policy Override Decisions
Providers who call the DAPO Center to request a PA for anti-obesity drugs or a policy override for other drugs or diabetic supplies are given an immediate decision about the PA or policy override, allowing members to receive drugs or diabetic supplies in a timely manner. The DAPO Center reviews PA requests and policy overrides for members enrolled in BadgerCare Plus, Wisconsin Medicaid, and SeniorCare.
Prior Authorization Requests
Prescribers or their billing providers are required to be enrolled in Wisconsin Medicaid to submit PA requests to ForwardHealth. Prescribers who are enrolled in Wisconsin Medicaid should indicate their name and NPI as the billing provider on PA requests. Providers who are not enrolled in Wisconsin Medicaid should indicate the name and NPI of the Wisconsin Medicaid-enrolled billing provider (for example, clinic) with which they are affiliated on PA requests.
When a prescriber, or their designee, calls the DAPO Center, a pharmacy technician will ask them a series of questions based on the Prior Authorization Drug Attachment for Anti-Obesity Drugs form. The prescriber, or their designee, should have all PA information completed on the appropriate PA drug attachment form before calling the DAPO Center to obtain PA. DAPO Center staff will ask for the name of the caller and the caller's credentials. (Is the caller an RN, physician assistant, physician, certified medical assistant, or nurse practitioner?)
Generally by the end of the call, if clinical PA criteria are met, DAPO Center staff will approve the PA request based on the information provided by the caller. If the PA request for an anti-obesity drug is approved, a decision notice letter will be mailed to the prescribing provider. After a PA for an anti-obesity drug has been approved, the prescriber should send the prescription to the pharmacy, and the member can pick up the drug. The member does not need to wait for the prescriber to receive the decision notice to pick up the drug at the pharmacy.
Note: If the provider receives a decision notice letter for a drug for which they did not request PA, the provider should notify the DAPO Center within 14 days of receiving the letter to inactivate the PA.
If a prescriber or their designee calls the DAPO Center to request PA and the clinical criteria for the PA are not met, the caller will be informed that the PA request is not approved because it does not meet the clinical criteria. If the prescriber chooses to submit additional medical documentation for consideration, they may submit the PA request to ForwardHealth for review by a pharmacist. The prescriber is required to submit a PA/RF and the applicable PA drug attachment form with the additional medical documentation. Documentation may be submitted to ForwardHealth through the Portal or by fax or mail.
Providers with questions about pharmacy policies and procedures may continue to call Provider Services.
Policy Override Decisions
When calling the DAPO Center to request a policy override, the following information must be provided:
- Member information
- Provider information
- Prescription information
- The reason for the override request
Topic #455 Fax
Faxing of all PA requests to ForwardHealth may eliminate one to three days of mail time. The following are recommendations to avoid delays when faxing PA requests:
- Providers should follow the PA fax procedures.
- Providers should not fax the same PA request more than once.
- Providers should not fax and mail the same PA request. This causes delays in processing.
PA requests containing X-rays, dental molds, or photos as documentation must be mailed; they may not be faxed.
To help safeguard the confidentiality of member health care records, providers should include a fax transmittal form containing a confidentiality statement as a cover sheet to all faxed PA requests. The Prior Authorization Fax Cover Sheet includes a confidentiality statement and may be photocopied.
Providers are encouraged to retain copies of all PA requests and supporting documentation before submitting them to ForwardHealth.
Prior Authorization Fax Procedures
Providers may fax PA requests to ForwardHealth at 608-221-8616. PA requests sent to any fax number other than 608-221-8616 may result in processing delays.
When faxing PA requests to ForwardHealth, providers should follow the guidelines/procedures listed below.
Fax Transmittal Cover Sheet
The completed fax transmittal cover sheet must include the following:
- Date of the fax transmission
- Number of pages, including the cover sheet (The ForwardHealth fax clerk will contact the provider by fax or telephone if all the pages do not transmit.)
- Provider contact person and telephone number (The ForwardHealth fax clerk may contact the provider with any questions about the fax transmission.)
- Provider number
- Fax telephone number to which ForwardHealth may send its adjudication decision
- To: "ForwardHealth Prior Authorization"
- ForwardHealth's fax number at 608-221-8616 (PA requests sent to any other fax number may result in processing delays.)
- ForwardHealth's telephone numbers
For specific PA questions, providers should call Provider Services.
Incomplete Fax Transmissions
If the pages listed on the initial cover sheet do not all transmit (i.e., pages stuck together, the fax machine has jammed, or some other error has stopped the fax transmission), or if the PA request is missing information, providers will receive the following by fax from the ForwardHealth fax clerk:
- A cover sheet explaining why the PA request is being returned
- Part or all of the original incomplete fax that ForwardHealth received
If a PA request is returned to the provider due to faxing problems, providers should do the following:
- Attach a completed cover sheet with the number of pages of the fax.
- Resend the entire original fax transmission and the additional information requested by the fax clerk to 608-221-8616.
General Guidelines
When faxing information to ForwardHealth, providers should not reduce the size of the PA/RF or the PA/HIAS1 to fit on the bottom half of the cover page. This makes the PA request difficult to read and leaves no space for consultants to write a response if needed or to sign the request.
If a photocopy of the original PA request and attachments is faxed, the provider should make sure these copies are clear and legible. If the information is not clear, it will be returned to the provider.
If the provider does not indicate his or her fax number, ForwardHealth will mail the decision back to the provider.
ForwardHealth will attempt to fax a response to the PA request to a provider three times. If unsuccessful, the PA request will be mailed to the provider.
If providers are not sure if an entire fax was sent, they should call ForwardHealth's fax clerk at 608-224-6124, to inquire about the status of the fax.
Prior Authorization Request Deadlines
Faxing a PA request eliminates one to three days of mail time. However, the adjudication time of the PA request has not changed. All actions regarding PA requests are made within the predetermined time frames.
Faxed PA requests received after 1:00 p.m. will be considered as received the following business day. Faxed PA requests received on a Saturday, Sunday, or holiday will be processed on the next business day.
Avoid Duplicating Prior Authorization Requests
After faxing a PA request, providers should not send the original paperwork by mail. Mailing the original paperwork after faxing the PA request will create duplicate PA requests in the system and may result in a delay of several days to process the faxed PA request.
Refaxing a PA request before the previous PA request has been returned will also create duplicate PA requests and may result in delays.
Response Back from ForwardHealth
Once ForwardHealth reviews a PA request, ForwardHealth will fax one of three responses back to the provider:
- "Your approved, modified, or denied PA request(s) is attached."
- "Your PA request(s) requires additional information (see attached). Resubmit the entire PA request, including the attachments, with the requested additional information."
- "Your PA request(s) has missing pages and/or is illegible (see attached). Resubmit the entire PA request, including the attachments."
Resubmitting Prior Authorization Requests
When resubmitting a faxed PA request, providers are required to resubmit the faxed copy of the PA request, including attachments. This will allow the provider to obtain the earliest possible grant date for the PA request (apart from backdating for retroactive enrollment). If any attachments or additional information that was requested is received without the rest of the PA request, the information will be returned to the provider. Topic #458 ForwardHealth Portal Prior Authorization
Providers can use the PA features on the ForwardHealth Portal to do the following:
- Submit PA requests and amendments for all services that require PA.
- View or maintain a PA collaboration (for certain services only).
- Save a partially completed PA request and return at a later time to finish completing it.
- Upload PA attachments and additional supporting clinical documentation for PA requests.
- Receive decision notice letters and returned provider review letters.
- Correct returned PA requests and PA amendment requests.
- Change the status of a PA request from "Suspended" to "Pending."
- Submit additional supporting documentation for a PA request that is in "Suspended" or "Pending" status.
- Search and view previously submitted PA requests or saved PA requests.
- Print a PA cover sheet.
Submitting PA Requests and Amendment Requests
Providers can submit PA requests for all services that require PA to ForwardHealth via the secure Provider area of the Portal. To save time, providers can copy and paste information from plans of care and other medical documentation into the appropriate fields on the PA request. Except for those providers exempt from NPI requirements, NPI and related data are required on PA requests submitted via the Portal.
When completing PA attachments on the Portal, providers can take advantage of an Additional Information field at the end of the PA attachment that holds up to five pages of text that may be needed.
Providers may also submit amendment requests via the Portal for PA requests with a status of "Approved" or "Approved with Modifications."
View or Maintain a PA Collaboration (for Certain Services Only)
A PA collaborative will link two or more PA requests for the same member together so providers can easily see and maintain them. Providers may collaborate on PA request submissions and amendments that are submitted for certain services through the Portal.
Any of the following provider types may initiate or add a PA request to a collaborative:
- Physical therapists
- Occupational therapists
- Speech-language pathologists
- Home health agencies
- Personal care agencies
PA requests and amendments will continue to be reviewed individually, regardless of whether they are part of a PA collaborative or not. The denial or modification of one PA request will not impact other PA requests in the same collaborative.
Saving Partially Completed PA Requests
Providers do not have to complete PA requests in one session; they can save partially completed PA requests at any point after the Member Information page has been completed by clicking on the Save and Complete Later button, which is at the bottom of each page. There is no limit to how many times PA requests can be saved.
Providers can complete partially saved PA requests at a later time by logging in to the secure Provider area of the Portal, navigating to the Prior Authorization home page, and clicking on the Complete a Saved PA Request link. This link takes the provider to a Saved PA Requests page containing all of the provider's PA requests that have been saved.
Once on the Saved PA Requests page, providers can select a specific PA request and choose to either continue completing it or delete it.
Note: The ability to save partially completed PA requests is only applicable to new PA requests. Providers cannot save partially completed PA amendments or corrections to returned PA requests or amendments.
30 Calendar Days to Submit or Re-Save PA Requests
Providers must submit or re-save PA requests within 30 calendar days of the date the PA request was last saved. After 30 calendar days of inactivity, a PA request is automatically deleted, and the provider has to re-enter the entire PA request.
The Saved PA Requests page includes a list of deleted PA requests. This list is for information purposes only and includes saved PA requests that have been deleted due to inactivity (it does not include PA requests deleted by the provider). Neither providers nor ForwardHealth are able to retrieve PA requests that have been deleted.
Submitting Completed PA Requests
ForwardHealth's initial receipt of a PA request occurs when the PA request is submitted on the Portal. Normal backdating policy applies based on the date of initial receipt, not on the last saved date. Providers receive a confirmation of receipt along with a PA number once a PA request is submitted on the Portal.
PA Attachments on the Portal
Almost all PA request attachments can be completed and submitted on the Portal. When providers are completing PA requests, the Portal presents the necessary attachments needed for that PA request. For example, if a physician is completing a PA request for physician-administered drugs, the Portal will prompt a PA/PAD and display the form for the provider to complete. Certain PA attachments cannot be completed online or uploaded.
Providers may also upload an electronically completed version of the paper PA attachment form. However, when submitting a PA attachment electronically, ForwardHealth recommends completing the PA attachment online as opposed to uploading an electronically completed version of the paper attachment form to reduce the chances of the PA request being returned for clerical errors.
All PA request attachment forms are available on the Portal to download and print to submit by fax or mail.
Providers may also choose to submit their PA request on the Portal and mail or fax the PA attachment(s) and/or additional supporting documentation to ForwardHealth. If the PA attachment(s) are mailed or faxed, a system-generated Portal PA Cover Sheet must be printed and sent with the attachment to ForwardHealth for processing. Providers must list the attachment(s) on the Portal PA Cover Sheet. When ForwardHealth receives the PA attachment(s) by mail or fax, they will be matched up with the PA/RF that was completed on the Portal.
Note: If the cover sheet could not be generated while submitting the PA request due to technical difficulties, providers can print the cover sheet from the main Portal PA page.
Before submitting any PA request documents, providers should save or print a copy for their records. Once the PA request is submitted, it cannot be retrieved for further editing.
As a reminder, ForwardHealth does not mail back any PA request documents submitted by providers.
Additional Supporting Clinical Documentation
ForwardHealth accepts additional supporting clinical documentation when the information cannot be indicated on the required PA request forms and is pertinent for processing the PA request or PA amendment request. Providers have the following options for submitting additional supporting clinical information for PA requests or PA amendment requests:
- Upload electronically
- Mail
- Fax
Providers can choose to upload electronic supporting information through the Portal in the following formats:
- JPEG (.jpg or .jpeg)
- PDF (.pdf)
- Rich Text Format (.rtf)
- Text File (.txt)
- OrthoCAD (.3dm) (for dental providers)
JPEG files must be stored with a ".jpg" or ".jpeg" extension; text files must be stored with a ".txt" extension; rich text format files must be stored with an ".rtf" extension; and PDF files must be stored with a ".pdf" extension. Dental OrthoCAD files are stored with a ".3dm" extension.
Microsoft Word files (.docx or .doc) cannot be uploaded but can be saved and uploaded in Rich Text Format or Text File formats.
In addition, providers can also upload additional supporting clinical documentation via the Portal when:
- Correcting a PA request or PA amendment request that is in a "Returned — Provider Review" status.
- Submitting a PA amendment request.
If submitting supporting clinical information via mail or fax, providers are prompted to print a system-generated Portal PA Cover Sheet to be sent with the information to ForwardHealth for processing. Providers must list the additional supporting information on the Portal PA Cover Sheet.
ForwardHealth will return PA requests and PA amendments requests when the additional documentation could have been indicated on the PA/RF and PA attachments or when the pertinent information is difficult to find.
"Suspended" PA Requests
For PA requests in a "Suspended" status, the provider has the option to:
- Change a PA request status from "Suspended" to "Pending."
- Submit additional documentation for a PA request that is in "Suspended" or "Pending" status.
Changing a PA Request From "Suspended" to "Pending"
The provider has the option of changing a PA request status from "Suspended — Provider Sending Info" to "Pending" if the provider determines that additional information will not be submitted. Changing the status from "Suspended — Provider Sending Info" to "Pending" will allow the PA request to be processed without waiting for additional information to be submitted. The provider can change the status by searching for the suspended PA request, checking the box indicating that the PA request is ready for processing without additional documentation, and clicking the Submit button to allow the PA request to be processed by ForwardHealth. There is an optional free form text box, which allows providers to explain or comment on why the PA request can be processed.
Submitting Additional Supporting Clinical Documentation for a PA Request in "Suspended" or "Pending" Status
There is an Upload Documents for a PA link on the PA home page in the provider secured Home Page. By selecting that link, providers have the option of submitting additional supporting clinical documentation for a PA request that is in "Suspended" or "Pending" status. When submitting additional supporting clinical documentation for a PA request that is in "Suspended" status, providers can choose to have ForwardHealth begin processing the PA request or to keep the PA request suspended. PA requests in a "Pending" status are processed regardless.
Note: When the PA request is in a "Pending" status and the provider uploads additional supporting clinical documentation, there may be up to a four-hour delay before the documentation is available to ForwardHealth in the system. If the uploaded information was received after the PA request was processed and the PA request was returned for missing information, the provider may resubmit the PA request stating that the missing information was already uploaded. Topic #456 Mail
Any type of PA request may be submitted on paper. Providers may mail completed PA requests, amendments to PA requests, and requests to enddate a PA request to ForwardHealth at the following address:
ForwardHealth
Prior Authorization
Ste 88
313 Blettner Blvd
Madison WI 53784
Providers are encouraged to retain copies of all PA requests and supporting documentation before submitting them to ForwardHealth. Topic #4618 NCPDP Transactions
ForwardHealth accepts the following NCPDP Telecommunication Standard Version D.0 PA transactions: P2 reversal, P3 inquiry, and the P4 request. These transactions enable providers to reverse or inactivate a PA, inquire about PA status, or submit a PA
request.
Providers should work closely with their software vendors or information
technology staff and software user guides to ensure that electronic PAs are
submitted accurately according to the ForwardHealth Payer Sheet: National Council for Prescription Drug Programs Version D.0.
The following are descriptions and/or requirements for each type of NCPDP PA
transaction:
P2 Reversal
To reverse a PA (i.e., change the PA to an inactive status) using the P2 transaction, all of the following must be true:
- The provider is the original provider who submitted the PA.
- The PA is in one of the following statuses:
- Approved — The PA request was approved.
- Returned — Provider Review: The PA request was returned to the provider for correction or for additional information.
- Pending — Fiscal Agent Review: The PA request is being reviewed by the fiscal agent.
- Pending — State Review: The PA request is being reviewed by the state.
- Suspended — Provider Sending Information: The PA request was submitted via the ForwardHealth Portal and the provider indicated they will be sending additional supporting information on paper.
- None of the services on an approved PA have been used.
P3 Inquiry
Providers may inquire about PAs they have previously submitted and receive PA information from ForwardHealth by submitting a P3 inquiry transaction. ForwardHealth recommends indicating the PA number, if known, when submitting a P3 inquiry. If a PA number is not included on the P3 inquiry, the most recent matching PA number will be reported.
P4 Request
Providers may submit an initial PA request using the P4 request transaction; however, this will not result in a real-time approval. The P4 request transaction does not allow providers to submit the required clinical information needed to adjudicate the PA request.
After submitting a PA request via the P4 transaction, providers will receive a real-time response indicating whether the transaction is accepted or rejected. If the transaction is rejected, the response will indicate a reject reason(s), and providers can correct and submit a new PA request using the P4 transaction.
An accepted P4 transaction with a captured response status will include a PA number. The PA request will be placed in a status of "Pending — Fiscal Agent Review."
Uploading Additional Documentation
Once providers receive the PA number, they may upload additional documentation (e.g., the PA attachment, supporting clinical information) for the pending PA through the Portal.
After receiving the additional documentation, ForwardHealth will adjudicate the PA request and send the provider either a decision notice or a returned provider review letter.
Returned Provider Review Letter
Once the PA request is in a Pending — Fiscal Agent Review status, ForwardHealth will review the request and, if the additional documentation has not been submitted, will send providers a returned provider review letter indicating the information required to adjudicate the request. PA requests cannot be adjudicated until ForwardHealth receives the additional information.
After receiving a returned provider review letter, providers should submit the additional information through the Portal, fax, or mail if they have not already done so. Providers have 30 calendar days from the date on the returned provider review letter to submit the additional information or the PA request will become inactive. After a PA request has become inactive, providers can submit a new request using the P4 transaction. Topic #1416 STAT-PA
Most drugs do not require PA. For drugs that require PA, pharmacy providers may submit PA requests through the STAT-PA system, the ForwardHealth Portal, an NCPDP transaction, or on paper.
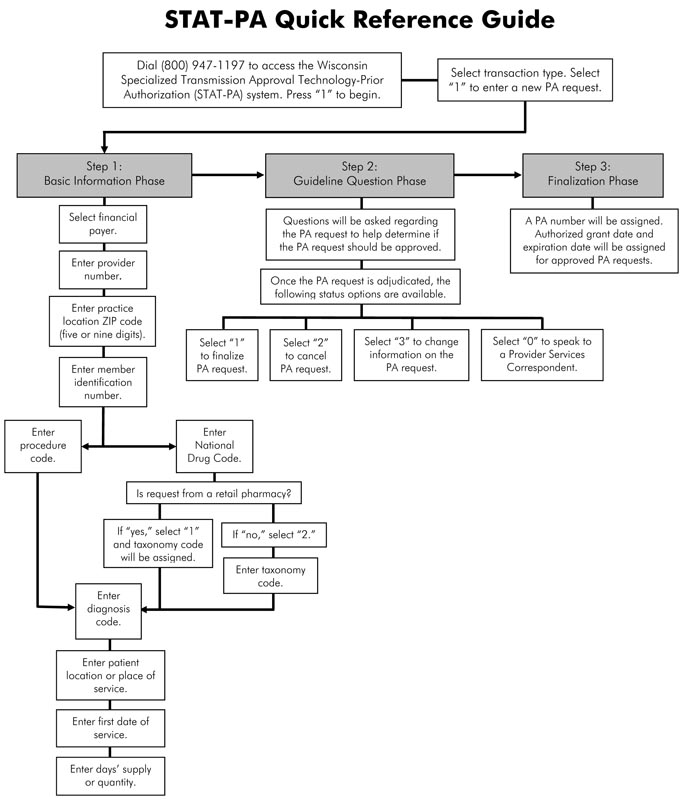
A STAT-PA Quick Reference Guide includes information about STAT-PA inquiries.
The STAT-PA system allows enrolled pharmacy providers to request and receive PA electronically, rather than on paper, for certain drugs. Providers are allowed to submit up to 24 PA requests per connection for touch-tone phone and Helpdesk queries. The STAT-PA system can be accessed using the STAT-PA System Instructions. The system is available 24 hours a day, seven days a week via phone at 800-947-1197.
STAT-PA Request Follow-Up
A STAT-PA request will either be approved or returned.
For STAT-PA requests that are approved, providers receive verbal confirmation of the approval at the end of the transaction. The verbal confirmation includes the following information:
- A PA number
- The grant date and expiration date
- The allowable days' supply
Providers are encouraged to write this information in the applicable fields of the PA drug attachment.
(Note: When a STAT-PA request is approved, the claim may be submitted immediately.)
For STAT-PA requests that are returned, providers receive the following information at the end of the transaction:
- A PA number
- The reason for the return
- A statement to submit the PA request with complete clinical documentation
Providers also receive a returned provider review letter by mail.
Reconsideration of a STAT-PA Request
Submit the following on paper for reconsideration of a STAT-PA request:
- A PA/RF. List the PA number assigned to the returned STAT-PA on the front of the PA/RF in the description field.
- An appropriate PA form.
- A fax number, if available.
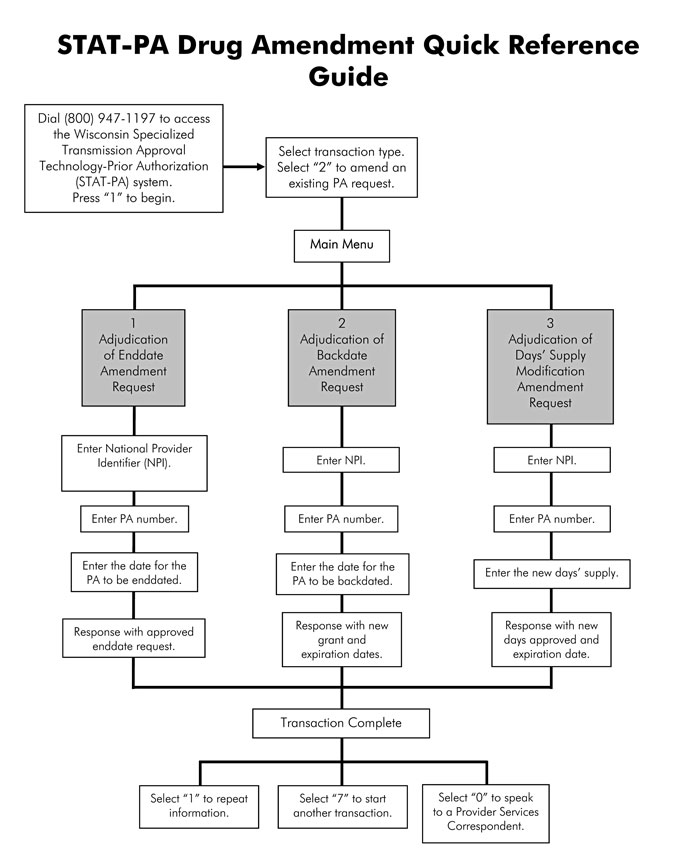
Amending Drug Prior Authorizations via STAT-PA
Providers may amend drug PAs that were initially approved through the STAT-PA system. Providers will be able to enddate, backdate, and change the quantity on an existing PA.
The following are requirements for each type of amendment.
Enddate a Prior Authorization via STAT-PA
Providers may enddate PAs using the STAT-PA system according to the following requirements:
- The PA must be for a drug.
- The provider must be the provider who obtained PA and must have the provider number used to obtain the PA.
- The PA must have been approved through STAT-PA initially.
- Prior authorization for the drug can be submitted through STAT-PA currently.
- The end date must be after the grant date and before the expiration date.
- The PA must not have been previously amended.
- The end date must be within 14 days of the current date.
- The end date must be within 29 days of the services (days' supply) that are already used on the PA.
Backdate a Prior Authorization via STAT‑PA
Providers can backdate up to 14 days prior to the date on which the PA was
initially submitted. To backdate a PA through STAT-PA, all of the following must
be true:
- The PA must be for a drug.
- The provider must be the provider who obtained PA and must have the provider number used to obtain the PA.
- The PA must have been approved through STAT-PA initially.
- PA for the drug can be submitted through STAT-PA currently.
- The backdate must be before the grant date.
- The PA must not have been previously amended.
- The backdated PA must not duplicate another PA.
Change the Days' Supply of a Prior Authorization via STAT-PA
To change the days' supply of a PA through STAT-PA, all of the following must
be true:
- The PA must be for a drug.
- The provider must be the provider who obtained PA and must have the provider number used to obtain the PA.
- The PA must have been approved through STAT-PA initially.
- PA for the drug can be submitted through STAT-PA currently.
- The PA must not have been previously amended.
- The change in days' supply must not duplicate another PA.
- The change in days' supply does not exceed the maximum allowed days' supply for the PA.
For STAT-PA amendment requests that are approved, providers receive verbal confirmation of the approval at the end of the transaction, as well as by mail.
If all of the criteria to amend a drug PA through STAT-PA cannot be met, providers may submit a PA amendment request on paper or via the Portal.
Dispensing STAT-PA Drugs When STAT-PA Is Unavailable
If the STAT-PA system is unavailable, a provider may still dispense a STAT-PA-approved drug. If a provider dispenses a new prescription for a STAT-PA-approved drug, the following steps must be taken:
- Obtain the member's ForwardHealth identification card, beige paper or white paper EE card, or SeniorCare identification card, and verify enrollment. Enrollment verification may be done by submitting a real-time claim for the drug or by using one of the other enrollment verification methods such as Wisconsin's EVS.
- Determine that the diagnosis is appropriate.
- Determine that the member is not taking any other drug in the same category. (The prospective DUR system may identify therapeutic duplications at other pharmacies.)
- Dispense up to a 14 days' supply of the drug.
- Request PA from the STAT-PA system when it is available. A PA request submitted using the STAT-PA system may be backdated up to 14 days using the STAT-PA system.
If a STAT-PA request is returned, submit a paper PA request within 14 days of dispensing along with documentation supporting what was done in steps 2 through 5 of this process.
 |