| Program Name: | BadgerCare Plus and Medicaid | Handbook Area: | Pharmacy | | 05/02/2024 | Prior Authorization : DecisionsTopic #4617 An Overview
ForwardHealth will make a decision regarding 24-hour PA requests, such as PA requests for brand medically necessary drugs, within 24 hours with the receipt of all the necessary information and telephone or fax the decision to the provider who submitted the PA request. Topic #424 Approved Requests
PA requests are approved for varying periods of time based on the clinical justification submitted. The provider receives a copy of a PA decision notice when a PA request for a service is approved. Providers may then begin providing the approved service on the grant date given.
An approved request means that the requested service, not necessarily the code, was approved. For example, a similar procedure code may be substituted for the originally requested procedure code. Providers are encouraged to review approved PA requests to confirm the services authorized and confirm the assigned grant and expiration dates.
Listing Procedure Codes Approved as a Group on the Decision Notice Letter
In certain circumstances, ForwardHealth will approve a PA request for a group
of procedure codes with a total quantity approved for the entire group. When
this occurs, the quantity approved for the entire group of codes will be
indicated with the first procedure code. All of the other approved procedure
codes within the group will indicate a quantity of zero.
Providers may submit claims for any combination of the procedure codes in the
group up to the approved quantity. Topic #4724 Communicating Prior Authorization Decisions
ForwardHealth will make a decision regarding a provider's PA request within 20 working days from the receipt of all the necessary information. After processing the PA request, ForwardHealth will send the provider either a decision notice letter or a returned provider review letter. Providers will receive a decision notice letter for PA requests that were approved, approved with modifications, or denied. Providers will receive a returned provider review letter for PA requests that require corrections or additional information. The decision notice letter or returned provider review letter will clearly indicate what is approved or what correction or additional information ForwardHealth needs to continue adjudicating the PA request.
Providers submitting PA requests via the ForwardHealth Portal will receive a decision notice letter or returned provider review letter via the Portal.
If the provider submitted a PA request via mail or fax and the provider has a Portal account, the decision notice letter or returned provider review letter will be sent to the provider via the Portal as well as by mail.
If the provider submitted a paper PA request via mail or fax and does not have a Portal account, the decision notice letter or returned provider review letter will be sent to the address indicated in the provider's file as their PA address (or to the physical address if there is no PA address on file), not to the address the provider wrote on the PA request.
The decision notice letter or returned provider review letter will not be faxed back to providers who submitted their paper PA request via fax. Providers who submitted their paper PA request via fax will receive the decision notice letter or returned provider letter via mail. Topic #5038 Correcting Returned Prior Authorization Requests and Request Amendments on the Portal
If a provider received a returned provider review letter or an amendment provider review letter, they will be able to correct the errors identified on the returned provider review letter directly on the ForwardHealth Portal. Once the provider has corrected the error(s), the provider can resubmit the PA request or amendment request via the Portal to ForwardHealth for processing. When correcting errors, providers only need to address the items identified in the returned provider review letter or the amendment provider review letter. Providers are not required to resubmit PA information already submitted to ForwardHealth. Topic #5037 Decision Notice Letters and Returned Provider Review Letters on the Portal
Providers can view PA decision notices and provider review letters via the secure area of the ForwardHealth Portal. Prior authorization decision notices and provider review letters can be viewed when the PA is selected on the Portal.
Note: The PA decision notice or the provider review letter will not be available until the day after the PA request is processed by ForwardHealth. Topic #425 Denied Requests
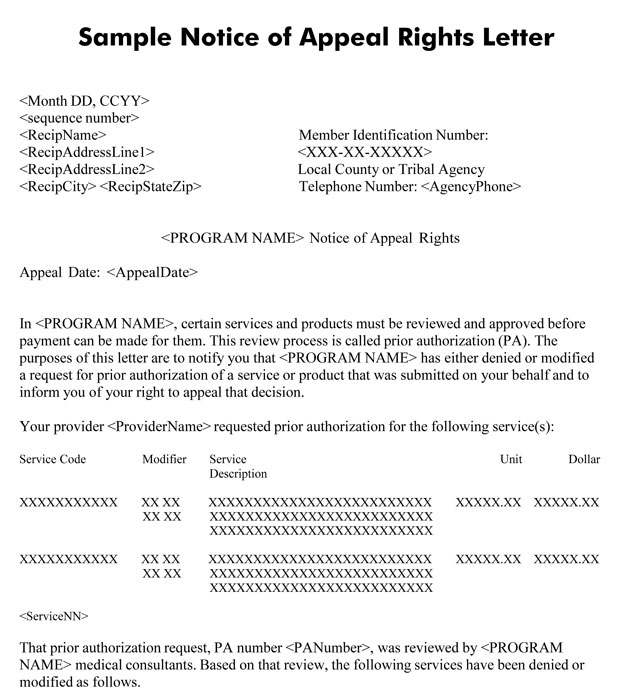
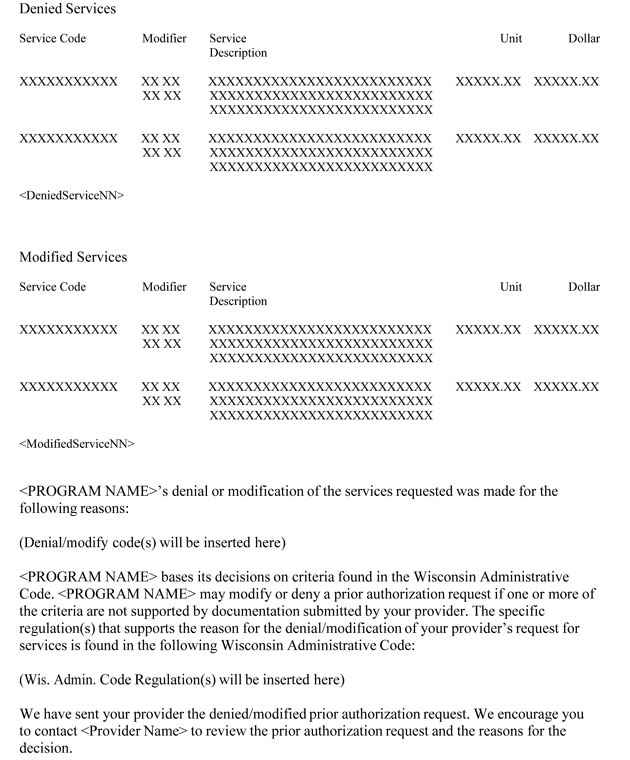
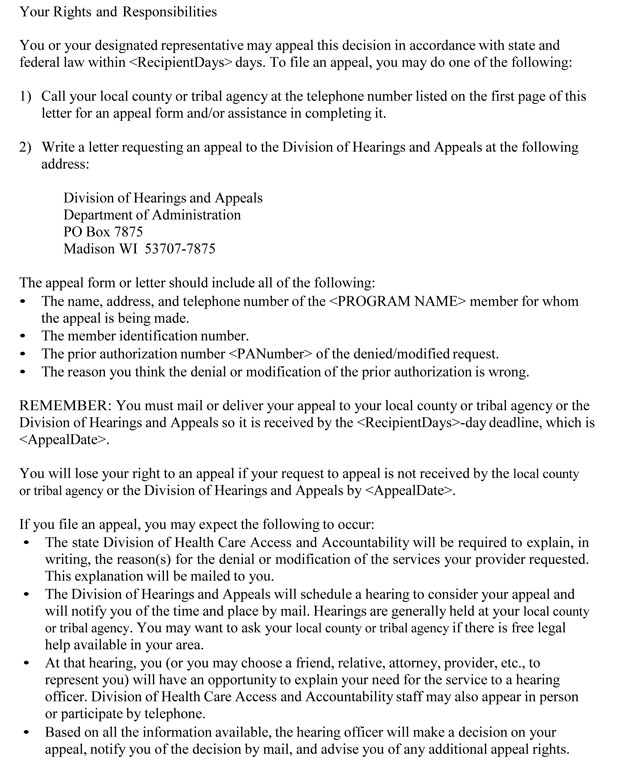
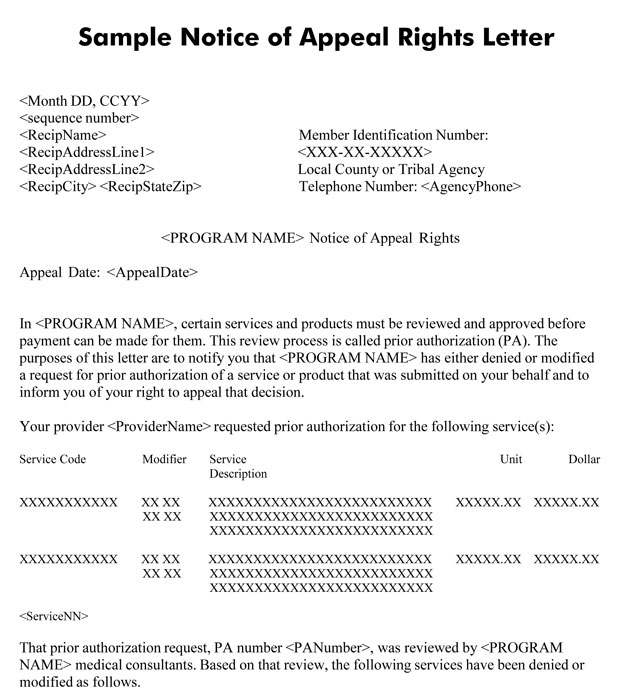
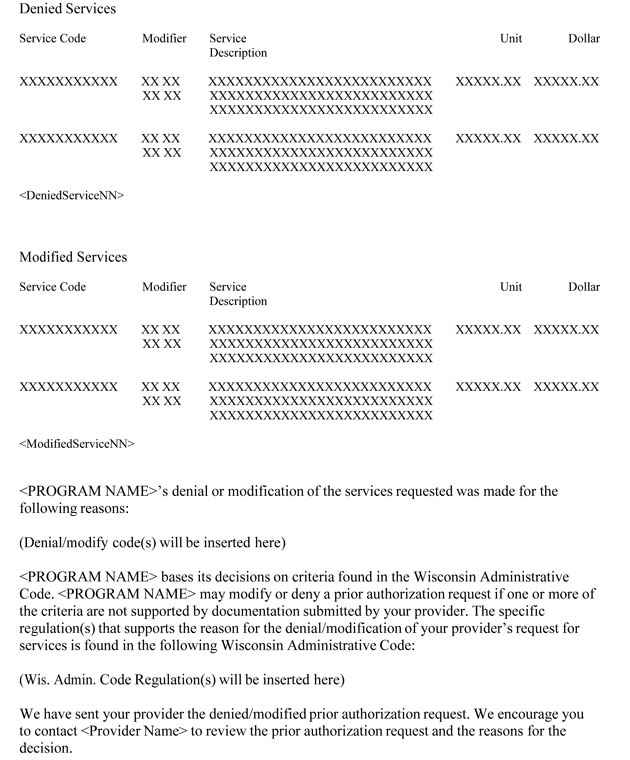
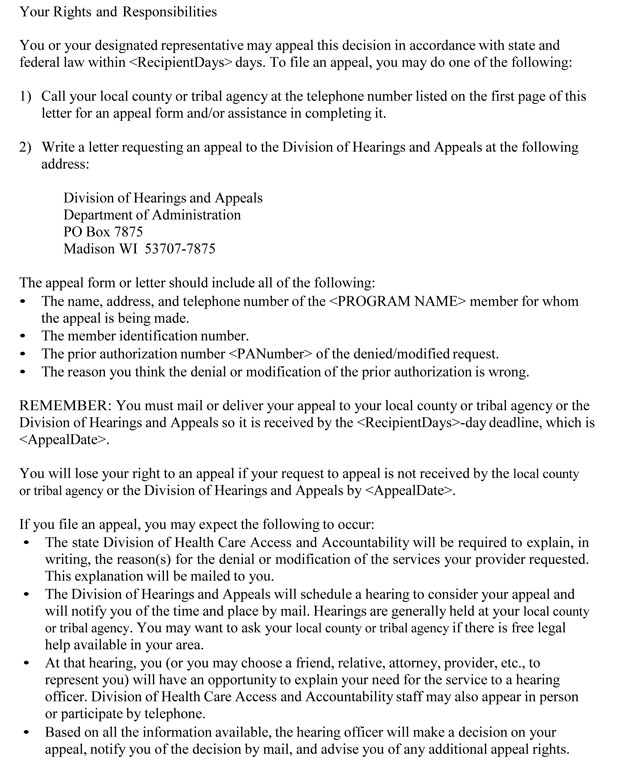
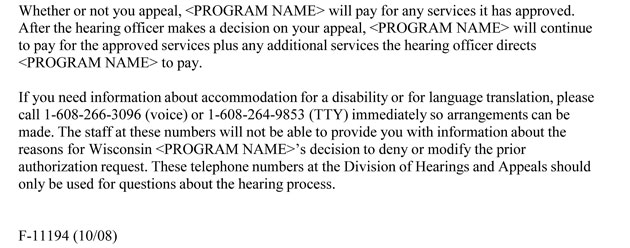
When a PA request is denied, both the provider and the member are notified. The provider receives a PA decision notice, including the reason for PA denial. The member receives a Notice of Appeal Rights letter that includes a brief statement of the reason PA was denied and information about their right to a fair hearing. Only the member, or authorized person acting on behalf of the member, can appeal the denial.
Providers may call Provider Services for clarification of why a PA request was denied.
Providers are required to discuss a denied PA request with the member and are encouraged to help the member understand the reason the PA request was denied.
Providers have three options when a PA request is denied:
- Not provide the service.
- Submit a new PA request. Providers are required to submit a copy of the original denied PA request and additional supporting clinical documentation and medical justification along with a new PA/RF, PA/DRF, or PA/HIAS1.
- Provide the service as a noncovered service.
If the member does not appeal the decision to deny the PA request or appeals the decision but the decision is upheld and the member chooses to receive the service anyway, the member may choose to receive the service(s) as a noncovered service.
 Topic #12837 Pharmacy Providers
If a PA is denied during adjudication, providers may submit a new request for the service using the P4 transaction; however, they are required to submit the original denied PA request, additional supporting clinical documentation, and medical justification via the Portal, fax, or mail following the submission guidelines. Topic #426 Modified Requests
Modification is a change in the services originally requested on a PA request. Modifications could include, but are not limited to, either of the following:
- The authorization of a procedure code different than the one originally requested.
- A change in the frequency or intensity of the service requested.
When a PA request is modified, both the provider and the member are notified. The provider will be sent a decision notice letter. The decision notice letter will clearly indicate what is approved or what correction or additional information is needed to continue adjudicating the PA request. The member receives a Notice of Appeal Rights letter that includes a brief statement of the reason PA was modified and information on their right to a fair hearing. Only the member, or authorized person acting on behalf of the member, can appeal the modification.
Providers are required to discuss with the member the reasons a PA request was modified.
Providers have the following options when a PA request is approved with modification:
- Provide the service as authorized.
- Submit a request to amend the modified PA request. Additional supporting clinical documentation and medical justification must be included.
- Not provide the service.
- Provide the service as originally requested as a noncovered service.
If the member does not appeal the decision to modify the PA request or appeals the decision but the decision is upheld and the member chooses to receive the originally requested service anyway, the member may choose to receive the service(s) as a noncovered service.
Providers may call Provider Services for clarification of why a PA request was modified.
 Topic #1324 Response Time
For most drugs, ForwardHealth responds by fax or telephone to the provider's paper PA request within 24 hours of the receipt of the request. The response consists of an acknowledgment that the PA request was received by ForwardHealth.
Weekend and Holiday Processing
Paper PA requests received Monday through Friday (except holidays) are handled as follows:
- If the request is received before 1 p.m. central time, ForwardHealth makes an attempt to notify the provider by telephone or fax within 24 hours.
- If the request is received after 1 p.m. central time, ForwardHealth makes an attempt to notify the provider by telephone or fax on the next regular business day.
Exceptions to the 24-Hour Response
ForwardHealth responds within 24 hours except when:
- The PA request contains insufficient, incorrect, or illegible information so that ForwardHealth cannot identify the requesting provider or determine that the requested service requires a 24-hour response.
- The PA request does not have the provider's telephone or fax number.
ForwardHealth makes three attempts to contact the provider by telephone or fax within 24 hours of receiving the PA request. Topic #4737 Returned Provider Review Letter Response Time
Thirty Days to Respond to the Returned Provider Review Letter
ForwardHealth must receive the provider's response within 30 calendar days of the date on the returned provider review letter, whether the letter was sent to
the provider by mail or through the ForwardHealth Portal. If the provider's response is received within 30 calendar days, ForwardHealth still considers the original
receipt date on the PA request when authorizing a grant date for the PA.
If ForwardHealth does not receive the provider's response within 30 calendar days of the date the returned provider review letter was sent, the PA status becomes inactive and the provider is required to submit a new PA request. This results in a later grant date if the PA request is approved. Providers will
not be notified when their PA request status changes to inactive, but this information will be available on the Portal and through WiCall.
If ForwardHealth receives additional information from the provider after the 30-day deadline has passed, a letter will be sent to the provider stating that the PA request is inactive and the provider is required to submit a new PA request. Topic #427 Returned Requests
A PA request may be returned to the provider when forms are incomplete, inaccurate, or additional clinical information or corrections are needed. When this occurs, the provider will be sent a provider review letter.
Returned Provider Review Letter
The returned provider review letter will indicate the PA number assigned to
the request and will specify corrections or additional information needed on the
PA request. Providers are required to make the corrections or supply the
requested information in the space provided on the letter or attach additional
information to the letter before mailing the letter to ForwardHealth. Providers
can also correct PAs that have been placed in returned provider review status in
the ForwardHealth Portal.
The provider's paper documents submitted with the PA request will not
be returned to the provider when corrections or additional information are
needed; however, X-rays and dental models will be returned once the PA is finalized.
Photographs submitted to ForwardHealth as additional supporting clinical documentation for PA requests will not be returned to providers and will be disposed of securely.
Therefore, providers are required to make a copy of their PA requests
(including attachments and any supplemental information) before mailing the
requests to ForwardHealth. The provider is required to have a copy on file for
reference purposes if more information is required about the PA
request.
Note: When changing or correcting the PA request, providers are reminded to
revise or update the documentation retained in their records. |