| Program Name: | BadgerCare Plus and Medicaid | Handbook Area: | Pharmacy | | 05/18/2024 | Covered and Noncovered Services : Medication Therapy ManagementTopic #14477 An Overview of Medication Therapy Management
ForwardHealth implemented the MTM benefit in conjunction with the WPQC. The MTM benefit consists of CMR/A services, which are private consultations between a pharmacist and a member to review the member's drug regimen. The member must be approved by ForwardHealth as a patient who is at high risk of experiencing medical complications due to their drug regimen to receive the CMR/A. The pharmacy requests approval to perform the CMR/A by calling the DAPO Center. In addition to Medicaid enrollment, WPQC certification is required to perform and receive reimbursement for CMR/A services. Topic #15177 Claims for SeniorCare Members With Spenddowns and Deductibles
State law limits what pharmacies may charge SeniorCare members for covered MTM services. Regardless of a member's level of participation in SeniorCare, pharmacies should always submit their usual and customary charge for MTM services, including services billed with procedure code 99607, if applicable. SeniorCare will track and maintain the member spenddown or deductible amounts for claims for MTM services. SeniorCare will inform the pharmacy of the amount to charge the member through the remittance information.
A pharmacy provider should never charge a member more than the amount indicated by SeniorCare, according to Wis. Stat. § 49.688(5)(a). If a SeniorCare member pays an amount greater than the amount on the remittance, the provider is required to refund the difference to the member.
Until a member meets any required spenddown, pharmacies may charge the member no more than their usual and customary rate for covered MTM services. Until a member meets any required deductible, pharmacies may charge the member no more than the Medicaid rate for covered MTM services.
Providers may obtain deductible and spenddown information for a specific member through the following sources:
- Remittance information
- Enrollment Verification on the ForwardHealth Portal
- Provider Services
SeniorCare Members at Level 2a (Deductible) Participation
Under level 2a (deductible) participation, a member is required to pay a $500 deductible in each of the following situations:
- Upon applying for SeniorCare, if the member meets the income limits for level 2a
- Subsequent to applying for SeniorCare, if the member meets the SeniorCare spenddown requirement
Until a member meets the required deductible, pharmacies may charge the member no more than the Medicaid rate for covered MTM services.
Dollars applied toward the deductible are not carried over into the next benefit period. After the member meets the deductible amount, the pharmacy may be reimbursed by Wisconsin Medicaid for covered MTM services.
SeniorCare Members at Level 2b (Deductible) Participation
Under level 2b (deductible) participation, a member is required to pay an $850 deductible in each of the following situations:
- Upon applying for SeniorCare, if the member meets the income limits for level 2b
- Subsequent to applying for SeniorCare, if the member meets the SeniorCare spenddown requirement
Until a member meets the required deductible, pharmacies may charge the member no more than the Medicaid rate for covered MTM services.
Dollars applied toward the deductible are not carried over into the next benefit period. After the member meets the deductible amount, the pharmacy may be reimbursed by Wisconsin Medicaid for covered MTM services.
SeniorCare Members at Level 3 (Spenddown) Participation
Under level 3 (spenddown) participation, members are required to pay a spenddown equal to the amount that their income exceeds 240 percent of the FPL. For households in which only one individual is eligible for SeniorCare, the member's spenddown amount is based on the individual's income. If the individual is married and living with their spouse, however, SeniorCare eligibility is based on the income of both spouses.
If both spouses are eligible for SeniorCare, the spenddown amount is based on the total of both members' incomes. SeniorCare-covered MTM services for either member will be applied to satisfy the spenddown amount.
Until a member meets any required spenddown, pharmacies may charge the member no more than their usual and customary rate for covered MTM services.
Dollars applied toward spenddown are not carried over into the next benefit period. After the member meets the spenddown amount, they must then meet the $850 deductible. Once the deductible is met, the pharmacy may be reimbursed by Wisconsin Medicaid for covered MTM services. Topic #14677 Comprehensive Medication Review and Assessments
ForwardHealth implemented the MTM benefit in conjunction with the WPQC. The MTM benefit consists of CMR/As.
The CMR/A services are voluntary medication reviews for members performed by a pharmacist. CMR/As may include one or more of the following analytical, consultative, educational, and monitoring services, provided by a pharmacist to help members get the best results from medications through enhancing consumer understanding of medication therapy, increasing adherence to medications, controlling costs, and preventing drug complications, conflicts, and interactions.
An initial face-to-face CMR/A identifies, resolves, and prevents medication-related problems, including adverse drug events, or can include performing medication reconciliation for a member discharged from a hospital or long-term care setting.
A follow up CMR/A monitors and evaluates the member's response to therapy, including safety and effectiveness of target medications.
Certification Requirements for Providing Comprehensive Medication Review and Assessments
To perform and be reimbursed for CMR/As, the pharmacists and the pharmacy at which a pharmacist is performing the CMR/A are required to be certified by an approved MTM program. Currently, the only approved MTM certification program is offered by the WPQC. The PSW manages the WPQC training and certification process, and has established rates for WPQC certification.
Conducting a Comprehensive Medication Review and Assessment
The CMR/A services may include the following value-added professional services provided by a pharmacist:
- Obtaining the necessary assessments of the member's health status.
- Formulating a medication treatment plan for the member.
- Providing an updated personal medication record and medication action plan for the member following each CMR/A visit.
- Providing information, support services, and resources designed to enhance member adherence with the therapeutic regimen.
- Providing verbal education and training designed to enhance the member's understanding and appropriate use of the medication.
- Documenting the care delivered and communicating essential information to the member's primary care providers.
- Referring to an appropriate health care provider, if necessary.
- Coordinating and integrating medication management services within the broader health care system.
- Notifying appropriate prescribers of each comprehensive care review and assessment service provided and sending a copy of the personal medication record and medication action plan. If authorizations to change specific medications are needed, the specific prescriber will be notified.
Qualifying Criteria for Members
A CMR/A service may be provided to a member who is at a high risk of experiencing medical complications due to their drug regimen. A high-risk member meets one of the following criteria:
- The member takes four or more prescription medications to treat or prevent two or more chronic conditions, one of which must be hypertension, asthma, chronic kidney disease, congestive heart failure, dyslipidemia, COPD, or depression.
- The member has diabetes.
- The member requires coordination of care due to multiple prescribers.
- The member has been discharged from a hospital or long-term care setting within the past 14 days; these services are referred to as transition of care CMR/A services.
- The member has health literacy issues as determined by the pharmacist.
- The member has been referred for the MTM services by the prescriber.
Members residing in a nursing home are not eligible for CMR/As.
If the member meets at least one of the aforementioned criteria, the pharmacy must call the DAPO Center to request approval to provide CMR/A services. The CMR/A approval covers the initial and up to three follow-up CMR/As.
Comprehensive Medication Review and Assessment Process
The following is a step-by-step process for providing a CMR/A:
- The pharmacist identifies an opportunity or receives a prescriber referral to perform a CMR/A.
- The pharmacy contacts the member about the CMR/A opportunity and the member accepts services.
- The pharmacy calls the DAPO Center to request approval to schedule a CMR/A.
- If approved, the pharmacist schedules an appointment with the member to perform the CMR/A.
- The pharmacist performs the CMR/A, which may include the following:
- Meeting with the member
- Consulting with the prescriber if needed
- Documenting the intervention
- The pharmacy submits a professional claim for the CMR/A.
Conducting Transition of Care Comprehensive Medication Review and Assessment Services
ForwardHealth expects the pharmacist to complete the following steps when rendering transition of care CMR/A services:
- Obtain a complete list of the prescription and over-the-counter medications, vitamins, and supplements the member was taking prior to admission to the hospital or long-term care setting. (If the pharmacist performing the service does not have a complete pre-admission medication list, the pharmacist should contact the member's pharmacy/pharmacies to obtain this information. An admission history obtained from an Electronic Medical Record does not fulfill this step requirement.)
- Obtain the discharge medication orders and compare to the pre-admission medication list.
- Upon conclusion of the CMR/A service, provide an updated medication list to the member that calls attention to changes made to the member's pre-admission medication regimen.
- Provide a MAP to the member that reminds the member of action items they should take until following up with their primary care provider. The final MAP should be provided to the member within 14 days of consultation.
- Maintain documentation in the member's file of the transition of care CMR/A services provided and submit required documentation electronically to ForwardHealth.
- Attempt to contact the member after the visit to ensure and reinforce understanding of the post-discharge medication regimen.
Note: Providers are reminded that PA from the DAPO Center is required in order to be reimbursed for providing transition of care CMR/A services.
Coordination of Benefits
Other health insurance sources also have MTM programs. If a member is eligible for another health insurance MTM program, the pharmacy provider is required to submit the claim to the member's other health insurance before submitting the claim to ForwardHealth.
Pharmacies are responsible for MTM COB. ForwardHealth is the payer of last resort.
The 1500 Health Insurance Claim Form Completion Instructions contain information regarding documenting other insurance information. Topic #14757 Comprehensive Medication Review and Assessments — Claim Submission
Claims for CMR/As must be submitted fee-for-service on a professional claim. In order to be reimbursed for a CMR/A, the pharmacy must submit a professional claim using a valid CPT code and modifier via one of the following claim submission methods:
- 837 transaction
- PES software
- DDE on the FowardHealth Portal
- 1500 Health Insurance Claim Form
ForwardHealth reduces reimbursement on most claims submitted to ForwardHealth on paper. Most paper claims are subject to up to a $1.10 reimbursement reduction per claim.
To ensure that members receive their CMR/A services in a timely manner, pharmacy providers are encouraged to schedule, perform, and submit claims for CMR/A services as soon as possible following approval of the CMR/A request. The submission of the claim is the indication to ForwardHealth that the service has been performed. The DAPO Center may inactivate the approval for a CMR/A service if it is not billed within the 60-day approval window.
Quantity on Claims for Initial and Follow-up Comprehensive Medication Reviews and Assessments
When submitting claims for an initial CMR/A, pharmacies should indicate CPT code 99605 with the modifier UA, with a quantity of "1" for the first 15 minutes. If the initial CMR/A lasts longer than 15 minutes, pharmacies should also indicate CPT code 99607 with modifier UA for each additional 15 minutes.
When submitting claims for a follow-up CMR/A, pharmacies should indicate CPT code 99606 with modifier UB, with a quantity of "1" for the first 15 minutes. If a follow-up CMR/A lasts longer than 15 minutes, pharmacies should indicate CPT code 99607 with modifier UB for each additional 15 minutes.
Pharmacies should note the following when submitting claims for each additional 15 minutes of a CMR/A using CPT code 99607:
- Procedure code 99607 must be listed on a separate detail line from the primary service code on claims for CMR/A services.
- Each claim detail must include the appropriate modifier.
- On the claim detail, each 15 minutes is equal to one unit (e.g., 30 minutes equals two units, 45 minutes equals three units, etc.). Providers should round up to the nearest 15 minutes when determining the number of units to bill. For example, if a CMR/A lasts 21 minutes, pharmacies should round to 30 minutes on the claim.
- The claim detail should be submitted with a zero dollar amount. (Claim details for procedure code 99607 are paid $0 since reimbursement for CMR/A services occurs with procedure code 99605 or 99606.)
Claim details for procedure code 99607 that are billed with a zero dollar amount are placed in a "pay" status with an amount paid of $0.
Although procedure code 99607 will be reimbursed at zero dollars, pharmacies must submit details with the correct quantities to comply with correct coding practices.
Determination of New or Established Patient Status
When submitting claims for MTM services, pharmacies should note that a new patient is one who has not received any MTM services from the pharmacy within the past three years. An established patient is one who has received MTM services from the pharmacy within the past three years. The CPT procedure code that a provider uses to bill the first 15 minutes of an MTM service indicates whether the member is a new (procedure code 99605) or an established (procedure code 99606) patient.
Providers billing multiple MTM services for any one member on the same DOS are reminded to use the appropriate CPT procedure code for that DOS. Claims will be denied if the member is indicated as both a new patient and an established patient on the same DOS.
Note: The DOS is defined as the date the medication was dispensed, if applicable (e.g., for a cost-effectiveness intervention), or the date the member received the MTM service (e.g., for a medication deletion intervention). Topic #14697 Comprehensive Medication Review and Assessments — Documentation Requirements
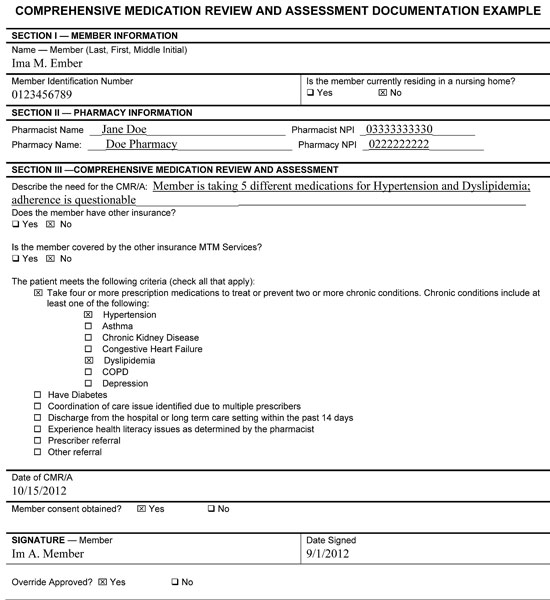
The following documentation is required for CMR/A services and must be maintained by the pharmacy in the member's file:
- Member information.
- Member name
- Member identification number
- Whether or not the member resides in a nursing home
- Pharmacist name and NPI.
- Pharmacy name and NPI.
- Description of the need for the CMR/A.
- Indication if the member has other insurance. If so, indicate whether or not the member is enrolled in the other insurance's MTM program.
- Indication of how the member meets the criteria to receive a CMR/A.
- Date of the CMR/A.
- Member consent for the CMR/A, indicated by the member's signature and date.
- Indication that DAPO approval was received for the CMR/A.
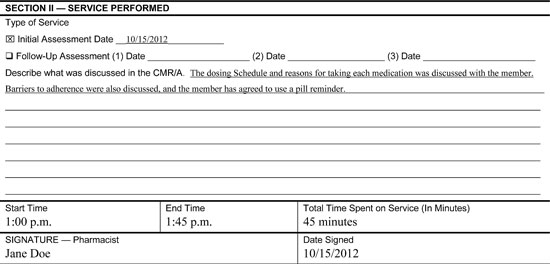
- Indication if this was the initial assessment or a follow-up assessment.
- Description of what was discussed in the CMR/A.
- Face-to-face start and end time of the CMR/A.
- Total time spent providing the CMR/A, including administrative time (however, administrative time should not be billed and will not be reimbursed).
- Pharmacist signature and date on the documentation.
Pharmacies may use any format to document CMR/As, but that format must include all of the aforementioned elements. Documentation must be made available to ForwardHealth upon request. Refer to the sample of acceptable documentation for CMR/A.
ForwardHealth also requires providers to submit MTM documentation electronically using one of the following options:
- ForwardHealth-approved MTM case management software
- The ForwardHealth Portal
This electronic submission requirement is in addition to the requirement for providers to maintain on-site MTM documentation (either on paper or electronically) in the member's file. The information required to be submitted to ForwardHealth electronically is the same information required to be maintained in the member's file. Documentation for MTM services that is submitted to ForwardHealth may be used by ForwardHealth to evaluate the MTM benefit.
Comprehensive Medication Review and Assessment Approval Process
Pharmacies are required to receive DAPO approval before scheduling a CMR/A with a member. Pharmacies may contact the DAPO Center from 8:00 a.m. to 5:30 p.m., Monday through Friday, except holidays.
When calling the DAPO Center for approval to schedule the CMR/A, the following information, similar to the documentation requirements, must be provided:
- Member information
- Pharmacy and pharmacist information
- Reason for the CMR/A
- Whether or not the member is enrolled in Medicare Part D
- Member's qualifying criteria
- Whether or not member consent was obtained
The member's verbal consent is required before calling the DAPO Center to request approval to schedule a CMR/A. The member's written consent (i.e., their signature) must be obtained before performing the CMR/A. If the member is a child or has physical or cognitive impairments that preclude the member from managing their own medications, a caregiver (e.g., caretaker relative, legal guardian, power of attorney, licensed health professional) may provide verbal or written consent on the member's behalf.
Generally DAPO Center staff will approve the CMR/A request by the end of the call based on the information provided by the caller. The pharmacy then must schedule, perform, and submit the claim for the CMR/A within 60 days following the approval. If the CMR/A is not provided within 60 days of approval, a new approval may be granted for a new pharmacy. The CMR/A approval is for the initial CMR/A and the three follow-up CMR/As.
If a pharmacy calls the DAPO Center to request CMR/A approval and the information provided does not qualify, the pharmacy will be informed that the request is not approved.
 Topic #14717 Comprehensive Medication Review and Assessments — Limitations
In most cases, a CMR/A is limited to one initial assessment and three follow-up assessments per rolling year.
Policy Override to Exceed Comprehensive Medication Review and Assessment Limitations
If a member requires more than the one initial and three follow-up CMR/As per rolling year (for example, a member is discharged from the hospital, released from long-term care, or has moved), pharmacies must contact the DAPO Center to request a policy override. Topic #14737 Comprehensive Medication Review and Assessments — Procedure Codes and Modifiers
Claims submitted for CMR/As must be submitted with at least one of the following CPT procedure codes:
- 99605—Medication therapy management service(s) provided by a pharmacist, individual, face-to-face with patient, with assessment and intervention if provided; initial 15 minutes, new patient.
- 99606—Medication therapy management service(s) provided by a pharmacist, individual, face-to-face with patient with assessment and intervention if provided; initial 15 minutes, established patient.
- 99607—Medication therapy management service(s) provided by a pharmacist, individual, face-to-face with patient, with assessment and intervention if provided; each additional 15 minutes (List separately in addition to code for primary service).
Procedure codes submitted for CMR/As must be submitted with one of the following modifiers:
- UA—The initial assessment of a member who is at high risk of experiencing medical complications due to their drug regimen.
- UB—Follow-up assessment of a member who experiencing medical complications due to their drug regimen and has already received an initial assessment by the pharmacy. The follow-up assessment will not be reimbursed unless the initial assessment has been reimbursed.
Pharmacists should submit one procedure code and modifier per detail line. Claim details without the appropriate modifier will be denied.
Comprehensive Medication Review and Assessment Procedure Codes and Modifiers
| Type of Comprehensive Medication Review and Assessment |
Description |
Modifier |
CPT Code for New Patient |
CPT Code for Established Patient |
Reimbursement |
Payable for nursing home residents? |
Limit |
| CMR/A—Initial Assessment |
This is an initial assessment of a member who is at a high risk of experiencing medical complications due to his drug regimen. |
UA | 99605 for first 15 minutes; 99607 for each additional 15 minutes |
99606 for first 15 minutes; 99607 for each additional 15 minutes | $85.00 |
No |
1/member/ rolling year |
| CMR/A—Follow-Up Assessment |
This is a follow-up assessment of a member who is at a high risk of experiencing medical complications due to the drug regimen and has already received an initial assessment by the pharmacy. |
UB |
N/A |
99606 for first 15 minutes; 99607 for each additional 15 minutes |
$40.00 |
No |
3/member/ rolling year |
Topic #14777 Comprehensive Medication Review and Assessments — Reimbursement
Pharmacies will be reimbursed at $85.00 for the initial CMR/A and $40.00 for a follow-up CMR/A.
For SeniorCare members, pharmacies are reimbursed directly for CMR/As at the Medicaid rate when the member is in, or has reached, the copayment level of participation. When the member has a spenddown or deductible, the pharmacy is reimbursed by the member. As a reminder, the pharmacy must obtain member consent for the CMR/A prior to providing the service.
Note: For a pharmacy to receive reimbursement for a CMR/A, the member must be enrolled in one of the covered programs on the DOS. Pharmacies are responsible for verifying the member's enrollment. Topic #17297 Electronic Submission of Documentation Requirement and Submission Options
ForwardHealth requires providers to submit MTM documentation electronically using one of the following options:
- ForwardHealth-approved MTM case management software
- The ForwardHealth Portal
This electronic submission requirement is in addition to the requirement for providers to maintain on-site MTM documentation (either on paper or electronically) in the member's file. The information required to be submitted to ForwardHealth electronically is the same information required to be maintained in the member's file. Documentation for MTM services that is submitted to ForwardHealth may be used by ForwardHealth to evaluate the MTM benefit.
Providers are required to submit the associated MTM documentation electronically within 365 days of submitting the claim for MTM services. Providers are encouraged to submit associated MTM documentation electronically within 30 days of submitting the claim for MTM services provided.
A separate record is required for each MTM service provided. Providers are reminded to only submit one record for each service provided. Documentation that is stored in ForwardHealth-approved MTM case management software is automatically sent to ForwardHealth; documentation stored on the Portal is also automatically sent to ForwardHealth. In order to avoid duplication, providers should not record documentation for the same services on both the Portal and in ForwardHealth-approved MTM case management software.
ForwardHealth-Approved Case Management Software
ForwardHealth will approve MTM case management software that meets certain criteria to access ForwardHealth's claim information. Approved software will be able to do the following:
- Identify BadgerCare Plus, SeniorCare, and Wisconsin Medicaid members who are eligible for MTM services.
- Submit claims for MTM services on a pharmacy provider's behalf.
- Capture, store, and maintain clinical information, including the required documentation for CMR/A services, in a member's file.
- Exchange clinical information with ForwardHealth. ForwardHealth will use this clinical information to evaluate the MTM benefit.
A list of ForwardHealth-approved vendors and their contact information is available.
Contracting Options
Pharmacy providers may choose to do one of the following:
- Contract with a ForwardHealth-approved MTM case management software vendor. Pharmacy providers who contract with a ForwardHealth-approved MTM case management software vendor are still required to receive approval from the DAPO Center to provide CMR/A services.
- Contract with another MTM case management software vendor. Pharmacy providers who contract with an MTM case management software vendor not approved by ForwardHealth should note that the unapproved vendor will not be able to receive claim information from or exchange documentation with ForwardHealth.
- Not contract with any MTM case management software vendor. Pharmacy providers who do not contract with any MTM case management software vendor can still submit claims for MTM services and are still required to capture, store, and maintain required documentation in a member's file and to submit required documentation electronically.
Documentation on the ForwardHealth Portal
Pharmacy providers have the option to capture, retrieve, and submit required MTM documentation on the secure Provider area of the ForwardHealth Portal. This is an optional service for providers; however, it will fulfill ForwardHealth's electronic documentation submission requirement for MTM services.
For assistance regarding the submission of MTM documentation on the Portal, call the ForwardHealth Portal Helpdesk or refer to the Medication Therapy Management Documentation Storage User Guide. Topic #14537 Medication Therapy Management Coordination
Pharmacies are responsible for COB for CMR/A MTM services. Topic #15199 Medication Therapy Management Services — Face-to-Face with Member or Caregiver
MTM services must be provided face-to-face with the member. Providers should attempt to provide MTM services in person whenever possible, but audio-visual telehealth delivery is allowable in cases that better fit the circumstances of the member. If the member is a child or has physical or cognitive impairments that preclude the member from managing their own medications, MTM services may be provided face-to-face to a caregiver (for example, caretaker relative, legal guardian, power of attorney, licensed health professional) on the member's behalf. Topic #15198 Medication Therapy Management Services — Member Eligibility
The MTM benefit is covered for members enrolled in the following programs:
- BadgerCare Plus
- SeniorCare
- Wisconsin Medicaid
Note: MTM services are reimbursed fee-for-service for all eligible members, including those enrolled in state-contracted managed care organizations. Pharmacy providers should submit fee-for-service claims directly to ForwardHealth for reimbursement. Topic #14797 Information is available for DOS before October 1, 2023.
Medication Therapy Management Services—Place of Service Codes
The following POS codes are allowed for CMR/A services:
| Code |
Description |
| 01 |
Pharmacy |
| 02 |
Telehealth Provided Other Than in Patient's Home |
| 05 |
Indian Health Service Free-Standing Facility |
| 06 |
Indian Health Service Provider-Based Facility |
| 07 |
Tribal 638 Free-Standing Facility |
| 08 |
Tribal 638 Provider-Based Facility |
| 10 |
Telehealth Provided in Patient's Home |
| 11 |
Office |
| 12 |
Home |
| 13 |
Assisted Living Facility |
| 14 |
Group Home |
| 16 |
Temporary Lodging |
| 17 |
Walk-in Retail Health Clinic |
| 19 |
Off Campus—Outpatient Hospital |
| 22 |
On Campus—Outpatient Hospital* |
| 27 |
Outreach Site/Street |
| 31 |
Skilled Nursing Facility** |
| 32 |
Nursing Facility** |
| 49 |
Independent Clinic |
| 50 |
Federally Qualified Health Center |
| 54 |
Intermediate Care Facility/Individuals With Intellectual Disabilities** |
| 56 |
Psychiatric Residential Treatment Center |
| 57 |
Non-Residential Substance Abuse Treatment Facility |
| 71 |
Public Health Clinic |
| 72 |
Rural Health Clinic |
* When a pharmacist performs a CMR/A service in an on-campus outpatient hospital setting, ForwardHealth does not reimburse the facility charge.
** These POS codes are only allowed for cost-effectiveness, dose/dosage form/duration change, medication addition, and medication deletion. Topic #15197 Medication Therapy Management Services — Referrals
Any licensed health professional who is Medicaid-enrolled and authorized to prescribe drugs can be a referring provider for covered MTM services. |