| Program Name: | BadgerCare Plus and Medicaid | Handbook Area: | Home Health | | 05/21/2024 | Covered and Noncovered Services : CodesTopic #2164 Diagnosis Codes for Private Duty Nursing
ForwardHealth requires that all codes indicated on claims (and PA requests when applicable) including diagnosis codes, revenue codes, HCPCS codes, and CPT codes be valid codes. Claims received without valid diagnosis codes, revenue codes, and HCPCS or CPT codes will be denied; PA requests received without valid codes will be returned to the provider. Providers should refer to current national coding and billing manuals for information on valid code sets.
All claims for PDN services provided to ventilator-dependent members must list ICD diagnosis code Z99.11 (Dependence on respirator [ventilator] status) as the primary diagnosis code on the claim form. Wisconsin Medicaid will not reimburse claims for respiratory services without this code.
Claims for PDN services that do not include services provided to a ventilator-dependent member require a valid diagnosis code other than Z99.11 (Dependence on respirator [ventilator] status). Topic #1079 Modifiers
All PDN and home health providers are required to use nationally recognized modifiers with procedure codes on PA requests and claim forms. No more than four modifiers can be entered for each day on the UB-04 claim form.
Start-of-Shift Modifiers
Providers are required to use state-defined start of shift modifiers on claims for home health services and PDN services. Start-of-shift modifiers are not required on PA requests.
Providers should choose the start-of-shift modifier that most closely represents the time each shift began. For each day, enter the modifiers in the order of occurrence. If a single shift spans over midnight from one day to the next, providers are required to use two start-of-shift modifiers.
Professional Status Modifiers
For services to ventilator-dependent members, providers are required to use one of two nationally recognized modifiers to indicate the nurse's professional status. Professional status modifiers are required on PA requests and claims. Topic #2162 Place of Service
When submitting PA requests, providers are required to include a POS code. Providers should choose the most appropriate POS when requesting PA. The following table lists examples of nationally recognized, two-digit POS codes.
| POS Code |
Description |
| 03 |
School |
| 12 |
Home |
| 99 |
Other Place of Service |
Topic #2161 Prior Authorization Number
Each PA request is assigned a unique ten-digit number.
When the POC is updated at times other than requesting PA, including the PA number on the POC is optional. Including the PA number on a POC that is not being submitted with a PA request is optional. However, Wisconsin Medicaid recommends that providers include the PA number on the POC even when it is optional. A PA number has record keeping advantages for the providers on the case and will make the POC easier to reference in the future. Topic #2160 Procedure Code and Modifier Table
The following table lists the HCPCS and CPT procedure codes providers should use when submitting claims and PA requests. The table also lists the modifiers that apply to each procedure code.
Note: All influenza virus vaccine and pneumococcal vaccine CPT procedure codes are covered under home health. No state-defined modifiers or state-defined start-of-shift modifiers are required for these procedure codes. Refer to Home Vaccination and Community Vaccination Clinics for more information about influenza and pneumococcal virus vaccines.
| Procedure Code and Description (Limited to Medicaid-Covered Service) |
State-Defined Modifier |
State-Defined Start-of-Shift Modifier |
| 92507—Treatment of speech, language, voice, communication, and/or auditory processing disorder; individual [per visit]
[ForwardHealth guidance: Indicate for home health speech therapy.] |
None |
UJ—Night (12–5:59 a.m.)
UF—Morning (6–11:59 a.m.)
UG—Afternoon (12–5:59 p.m.)
UH—Evening (6–11:59 p.m.) |
| 97139—Unlisted therapeutic procedure (specify) [per visit]
[ForwardHealth guidance: Indicate for home health occupational therapy.] |
None |
UJ—Night (12–5:59 a.m.)
UF—Morning (6–11:59 a.m.)
UG—Afternoon (12–5:59 p.m.)
UH—Evening (6–11:59 p.m.) |
| 97799—Unlisted physical medicine/rehabilitation service or procedure [per visit]
[ForwardHealth guidance: Indicate for home health physical therapy.] |
None |
UJ—Night (12–5:59 a.m.)
UF—Morning (6–11:59 a.m.)
UG—Afternoon (12–5:59 p.m.)
UH—Evening (6–11:59 p.m.) |
| 99504—Home visit for mechanical ventilation care [per hour]
[ForwardHealth guidance: Indicate for private duty nurse—ventilation care.] |
TE—LPN/LVN |
UJ—Night (12–5:59 a.m.)
UF—Morning (6–11:59 a.m.)
UG—Afternoon (12–5:59 p.m.)
UH—Evening (6–11:59 p.m.) |
| 99504—Home visit for mechanical ventilation care [per hour]
[ForwardHealth guidance: Indicate for private duty nurse—ventilation care.] |
TD—RN |
UJ—Night (12–5:59 a.m.)
UF—Morning (6–11:59 a.m.)
UG —Afternoon (12–5:59 p.m.)
UH — Evening (6–11:59 p.m.) |
| 99600—Unlisted home visit service or procedure [per visit]
[ForwardHealth guidance: Indicate for home health intermittent skilled nursing visit.] |
None |
UJ—Night (12–5:59 a.m.)
UF—Morning (6–11:59 a.m.)
UG—Afternoon (12–5:59 p.m.)
UH—Evening (6–11:59 p.m.) |
| 99600—Unlisted home visit service or procedure [per visit]
[ForwardHealth guidance: Indicate for home health intermittent skilled nursing visit.] |
TS—Follow-up service |
UJ—Night (12–5:59 a.m.)
UF—Morning (6–11:59 a.m.)
UG—Afternoon (12–5:59 p.m.)
UH—Evening (6–11:59 p.m.) |
| S9123—Nursing care, in the home; by registered nurse, per hour
[ForwardHealth guidance: Indicate for private duty registered nurse.] |
None |
UJ—Night (12–5:59 a.m.)
UF—Morning (6–11:59 a.m.)
UG—Afternoon (12–5:59 p.m.)
UH—Evening (6–11:59 p.m.) |
| S9124—Nursing care, in the home; by licensed practical nurse, per hour
[ForwardHealth guidance: Indicate for private duty licensed practical nurse.] |
None |
UJ—Night (12–5:59 a.m.)
UF—Morning (6–11:59 a.m.)
UG—Afternoon (12–5:59 p.m.)
UH—Evening (6–11:59 p.m.) |
| T1001—Nursing assessment/evaluation [per visit] |
None |
UJ—Night (12–5:59 a.m.)
UF—Morning (6–11:59 a.m.)
UG—Afternoon (12–5:59 p.m.)
UH—Evening (6–11:59 p.m.) |
| T1021—Home health aide or certified nurse assistant, per visit |
None |
UJ—Night (12–5:59 a.m.)
UF—Morning (6–11:59 a.m.)
UG—Afternoon (12–5:59 p.m.)
UH—Evening (6–11:59 p.m.) |
| T1021—Home health aide or certified nurse assistant, per visit |
TS—Follow-up service |
UJ—Night (12–5:59 a.m.)
UF—Morning (6–11:59 a.m.)
UG—Afternoon (12–5:59 p.m.)
UH—Evening (6–11:59 p.m.) |
| T1502—Administration of oral, intramuscular and/or subcutaneous medication by health care agency/professional, per visit |
None |
UJ—Night (12–5:59 a.m.)
UF—Morning (6–11:59 a.m.)
UG—Afternoon (12–5:59 p.m.)
UH—Evening (6–11:59 p.m.) |
Topic #2159 Procedure Codes
When submitting PA requests and claims, home health providers should use HCPCS procedure codes. Providers should refer to the DME Index for a list of valid procedure codes for DME. Providers should refer to the DMS Index for a list of valid procedure codes for DMS.
Home health agencies providing PDN services to ventilator-dependent members should use CPT procedure codes on PA requests and claims. Topic #2158 Revenue Codes
Providers are required to use a revenue code when submitting claims to ForwardHealth. The following table contains a list of revenue code examples. Providers should use the appropriate revenue code that best describes the service performed.
For the most current and complete list of revenue codes, contact the AHA NUBC by calling 312-422-3390 or writing to the following address:
American Hospital Association National Uniform Billing Committee
29th Fl
1 N Franklin
Chicago IL 60606
For further information, refer to the NUBC website.
| Revenue Code |
Service Description |
| 0550 |
General Skilled Nursing |
| 0551 |
Skilled Nursing Visit |
| 0552 |
Skilled Nursing Hourly Charge |
| 0580 |
Other Home Health Services, Except Therapies |
| 0420 |
Physical Therapy |
| 0430 |
Occupational Therapy |
| 0440 |
Speech and Language Pathology |
Topic #2157 Units of Service
The number of services (visits or hours) billed must be listed on each detail line of the claim form.
Home health aide visits, home health skilled nursing visits, and home health therapy visits are billed as one unit of service per day. If the quantity billed is not an increment of a whole unit, the service is denied.
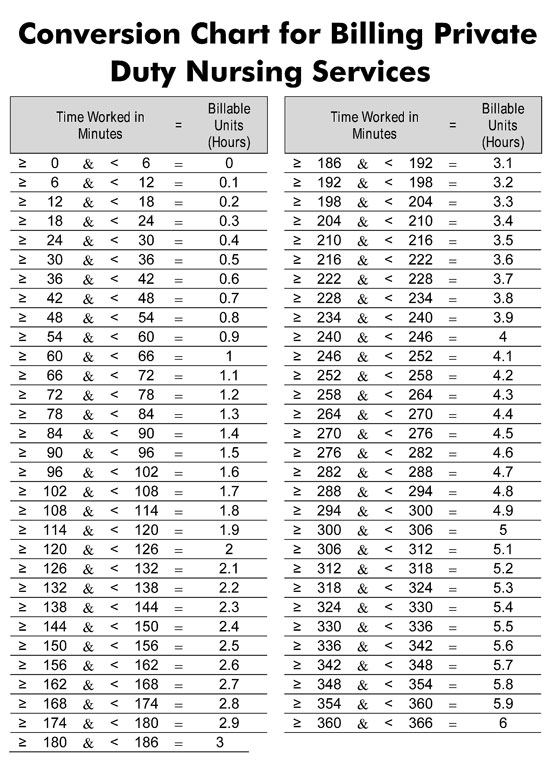
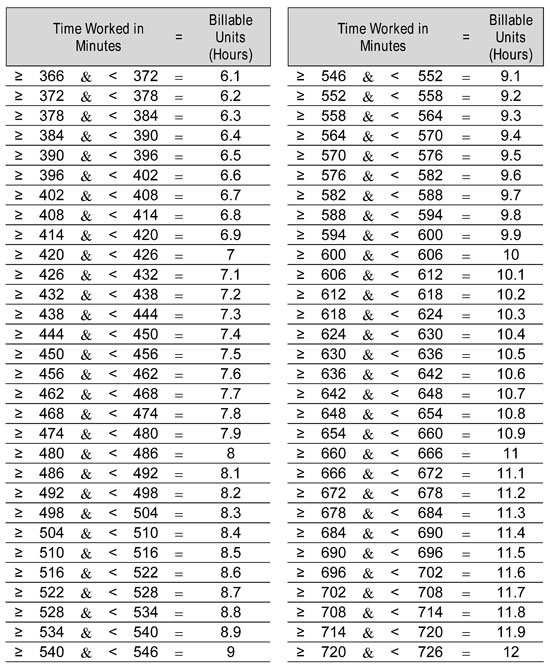
Providers are required to bill their PDN services in six-minute increments according to the conversion chart for billing PDN services. Services must be recorded as one tenth (0.1) of a unit. One unit equals one hour. Reimbursement is not available for less than six minutes of service. For example, a provider who works for seven hours and 55 minutes would bill 7.9 units.
 Topic #643 Unlisted Procedure Codes
According to the HCPCS codebook, if a service is provided that is not accurately described by other HCPCS CPT procedure codes, the service should be reported using an unlisted procedure code.
Before considering using an unlisted, or NOC, procedure code, a provider should determine if there is another more specific code that could be indicated to describe the procedure or service being performed/provided. If there is no more specific code available, the provider is required to submit the appropriate documentation, which could include a PA request, to justify use of the unlisted procedure code and to describe the procedure or service rendered. Submitting the proper documentation, which could include a PA request, may result in more timely claims processing.
Unlisted procedure codes should not be used to request adjusted reimbursement for a procedure for which there is a more specific code available.
Unlisted Codes That Do Not Require Prior Authorization or Additional Supporting Documentation
For a limited group of unlisted procedure codes, ForwardHealth has established specific policies for their use and associated reimbursement. These codes do not require PA or additional documentation to be submitted with the claim. Providers should refer to their service-specific area of the Online Handbook on the ForwardHealth Portal for details about these unlisted codes.
For most unlisted codes, ForwardHealth requires additional documentation.
Unlisted Codes That Require Prior Authorization
Certain unlisted procedure codes require PA. Providers should follow their service-specific PA instructions and documentation requirements for requesting PA. For a list of procedure codes for which ForwardHealth requires PA, refer to the service-specific interactive maximum allowable fee schedule.
In addition to a properly completed PA request, documentation submitted on the service-specific PA attachment or as additional supporting documentation with the PA request should provide the following information:
- Specifically identify or describe the name of the procedure/service being performed or billed under the unlisted code.
- List/justify why other codes are not appropriate.
- Include only relevant documentation.
- Include all required clinical/supporting documentation.
For most situations, once the provider has an approved PA request for the unlisted procedure code, there is no need to submit additional documentation along with the claim.
Unlisted Codes That Do Not Require Prior Authorization
If an unlisted procedure code does not require PA, documentation submitted with the claim to justify use of the unlisted code and to describe the procedure/service rendered must be sufficient to allow ForwardHealth to determine the nature and scope of the procedure and to determine whether or not the procedure is covered and was medically necessary, as defined in Wisconsin Administrative Code.
The documentation submitted should provide the following information related to the unlisted code:
- Specifically identify or describe the name of the procedure/service being performed or billed under the unlisted code.
- List/justify why other codes are not appropriate.
- Include only relevant documentation.
How to Submit Claims and Related Documentation
Claims including an unlisted procedure code and supporting documentation may be submitted to ForwardHealth in the following ways:
- If submitting on paper using the 1500 Health Insurance Claim Form, the provider may do either of the following:
- Include supporting information/description in Item Number 19 of the claim form.
- Include supporting documentation on a separate paper attachment. This option should be used if Item Number 19 on the 1500 Health Insurance Claim Form does not allow enough space for the description or when billing multiple unlisted procedure codes. Providers should indicate "See Attachment" in Item Number 19 of the claim form and send the supporting documentation along with the claim form.
- If submitting electronically using DDE on the Portal, PES software, or 837 electronic transactions, the provider may do one of the following:
- Include supporting documentation in the Notes field. The Notes field is limited to 80 characters.
- Indicate that supporting documentation will be submitted separately on paper. This option should be used if the Notes field does not allow enough space for the description or when billing multiple unlisted procedure codes. Providers should indicate "See Attachment" in the Notes field of the electronic transaction and submit the supporting documentation on paper.
- Upload claim attachments via the secure Provider area of the Portal.
Topic #830 Valid Codes Required on Claims
ForwardHealth requires that all codes indicated on claims and PA requests, including diagnosis codes, revenue codes, HCPCS codes, HIPPS codes, and CPT codes be valid codes. Claims received without valid diagnosis codes, revenue codes, and HCPCS, HIPPS, or CPT codes will be denied; PA requests received without valid codes will be returned to the provider. Providers should refer to current national coding and billing manuals for information on valid code sets.
Code Validity
In order for a code to be valid, it must reflect the highest number of required characters as indicated by its national coding and billing manual. If a stakeholder uses a code that is not valid, ForwardHealth will deny the claim or return the PA request, and it will need to be resubmitted with a valid code.
Code Specificity for Diagnosis
All codes allow a high level of detail for a condition. The level of detail for ICD diagnosis codes is expressed as the level of specificity. In order for a code to be valid, it must reflect the highest level of specificity (that is, contain the highest number of characters) required by the code set. For some codes, this could be as few as three characters. If a stakeholder uses an ICD diagnosis code that is not valid (that is, not to the specific number of characters required), ForwardHealth will deny the claim or return the PA request, and it will need to be resubmitted with a valid ICD diagnosis code. |