| Program Name: | BadgerCare Plus and Medicaid | Handbook Area: | Hearing | | 05/06/2024 | Prior Authorization : Services Requiring Prior AuthorizationTopic #2957 An Overview
The following services require PA:
- Aural rehabilitation:
- Use of residual hearing.
- Speech reading or lip reading.
- Compensation techniques.
- Gestural communication techniques.
- Purchase of any special modifications to hearing instruments.
- Purchase or rental of all hearing instruments.
- Replacement of any hearing instruments.
- SLP services. As stated in Wis. Admin. Code § DHS 107.18, SLP services provided by audiologists beyond the first 35 treatment days per spell of illness require PA. In addition, SLP services require PA requests specifically for spell of illness, Birth to 3, and therapy services.
- Unlisted otorhinolaryngological service or procedure.
BadgerCare Plus recognizes that a member's abilities, needs, and medical conditions are unique and have the potential to change. Therefore, approval of one PA does not guarantee approval of all PAs.
Conversely, a denied PA should not be interpreted to mean that services will not meet the definition of medical necessity in the future. Every PA request stands on its own merit, documenting the need for services and describing the member's unique circumstances at that time. Topic #19117 Audiology Professional Services
The following covered audiology professional services require PA:
- Aural rehabilitation
- SLP services (As stated in Wis. Admin. Code § DHS 107.18(2)(b), SLP services provided by audiologists beyond the first 35 treatment days per spell of illness require PA.)
Topic #18057 Bone-Anchored Hearing Device Repairs and Replacements
HCPCS procedure codes L7510 (Repair of prosthetic device, repair or replace minor parts) and L8691 (Auditory osseointegrated device, external sound processor excludes transducer/actuator; replacement only, each) are allowable for repairs and replacements of bone-anchored hearing devices.
PA is required for procedure code L7510 if the total repair of the bone-anchored hearing device exceeds $150.00 or if the replacement parts of the bone-anchored hearing device have not exceeded their life expectancy.
PA is not required for procedure code L8691.
Note: ForwardHealth assigns "U" modifiers to multiple items listed on PA requests to indicate separate approval of DME items (i.e., accessories). Topic #691 Cochlear Implants Repairs and Replacements
PA is required is required in the following circumstances:
- External speech processor needs to be replaced within three years of the implant surgery or a previous replacement
- Total cost for repair of the cochlear implant or parts of the implant (procedure code L7510) exceeds $150.00
- Replacement parts exceed life expectancy
ForwardHealth assigns "U" modifiers to multiple items listed on PA requests to indicate separate approval of DME items (i.e., accessories).
Note: Audiologists and speech and hearing clinics, as well as DME providers, may submit PA requests and submit claims for replacement parts and accessories. Topic #2955 Ear Molds and Impressions
For members under 18 years of age, three ear molds and impressions per hearing aid per year are allowed without PA. PA is required if more than three ear molds and impressions are needed per hearing aid per year.
For members 18 years of age and older, one ear mold and impression per hearing aid per year is allowed without PA. PA is required for more than one ear mold and impression per hearing aid per year. Topic #2984 Hearing Aid Replacement
Equipment Failure and Loss or Damage Under Warranty
If, within 24 months of purchase, persistent repairs are required due to equipment failure, the manufacturer may choose to replace the hearing aid at no cost to the provider, member, or Wisconsin Medicaid. No further reimbursement will be made for the replacement hearing aid. However, if the manufacturer chooses to replace the hearing aid after the original 12-month dispensing service guarantee has expired, Wisconsin Medicaid will reimburse the additional dispensing fee. PA is not required for replacing a hearing aid that is covered under the equipment warranty. It is also not required for the dispensing of the replacement hearing aid.
Additionally, if during the loss and damage warranty or the equipment warranty the manufacturer replaces a hearing aid, the new model must be equal to or better than the original model. The replacement must include a full 24-month equipment warranty, which begins the date the provider receives the hearing aid.
Loss or Irreparable Damage Not Under Warranty
If a hearing aid is lost or damaged beyond reasonable repair and is no longer covered under a loss and damage warranty, providers are encouraged to request PA from ForwardHealth for a replacement hearing aid. Replacing a lost or damaged hearing aid is not restricted by a hearing aid's life expectancy.
Providers are required to include the following with PA requests for replacement of lost or damaged hearing aids:
- The provider's statement that the hearing aid is not covered by a manufacturer's loss and damage warranty
- Information regarding instructions given to the member on care and maintenance of a hearing aid so that a hearing aid is not lost or damaged in the future
- A statement from the member or member's caregiver regarding how the hearing aid was lost and the steps taken to recover the hearing aid
- A statement from the member or member's caregiver that insurance (e.g., homeowners, property, renters) does not cover replacing the lost hearing aid, if applicable
Life Expectancy
If a hearing aid is no longer covered under warranty and needs to be replaced within five years of purchase (i.e., the hearing aid was purchased over 24 months ago but less than five years ago), PA is required for the replacement.
Dispensing and Fitting
Wisconsin Medicaid only reimburses providers for one dispensing fee per member, per ear, per 12-month period after the fitting of a hearing aid. Wisconsin Medicaid will not reimburse an additional dispensing fee if a hearing aid is replaced within 12 months of the original dispensing date. Providers are required to indicate on claims the HCPCS procedure code that most appropriately reflects the number of hearing devices dispensed.
Noncontracted Hearing Aid Styles
For noncontracted hearing aid styles, the manufacturer determines the trial period, loss and damage warranty, equipment warranty, and repair warranty. Topic #2951 Member Special Needs
A member's special educational, social, vocational, and other needs are considered when PA requests for hearing instruments are adjudicated. The audiologist is required to document a member's special needs in the PA request or in an attachment to the PA request. Examples of special needs include:
- Educational
- Allowing effective education for an adult or child who is mentally or physically impaired
- Allowing effective education of a child who is under the age of 21
- Social
- Enhancing a mentally or physically impaired member's social communication skills and abilities.
- Enhancing a mentally or physically impaired member's capability for sound awareness (localization), e.g., for parenting, warning
- Expanding a member's social interaction or communication limited by additional disabilities, such as blindness
- Vocational
- Improving a mentally or physically impaired member's ability to obtain employment or continue employment
Topic #2952 Monaural or Binaural Hearing Instruments
ForwardHealth requires the following information on the PA request for monaural or binaural hearing instruments:
- Complete description of the hearing device, including style, electroacoustic specifications, and any modifications and adaptations
- Complete documentation that supports the medical necessity of the request, including the diagnosis, appropriate audiological evaluation, and a description and diagnosis of any cognitive or behavioral impairments or other special needs
- Documentation that the medically necessary hearing tests and evaluations have been performed to confirm fitting of the monaural or binaural hearing instrument
- Member's primary and secondary diagnosis codes from the ICD that relate to a hearing problem or developmental, cognitive, or neurological condition
Topic #4516 Non-implant Bone-Anchored Hearing Devices
Non-implant bone-anchored hearing devices (HCPCS procedure code L8692) require PA. All of the following criteria must be met before PA requests for non-implant bone-anchored hearing devices can be approved:
- The member has a conductive and/or mixed hearing loss (unilateral or bilateral) with pure-tone average bone-conduction thresholds (measured at 0.5, 1, 2, and 3 kHz) less than or equal to 65 dB HL. The threshold range is intended to accommodate different degrees of hearing loss and corresponding output power of the bone-anchored hearing device.
- The member demonstrates an air-bone gap of at least 30 dB.
- The member demonstrates a word recognition score greater than 60 percent via conventional air-conduction speech audiometry using single-syllable words.
- The member has one or more of the following conditions:
- Severe chronic external otitis or otitis media
- Chronic draining ear through a tympanic membrane perforation
- Malformation of the external auditory canal or middle ear
- Stenosis of the external auditory canal
- Ossicular discontinuity or erosion that cannot be repaired
- Chronic dermatologic conditions such as psoriasis of the ear canal
- Tumors of the external canal and/or tympanic cavity
- Other conditions that prevent restoration of hearing using a conventional air-conduction hearing aid
When requesting PA for non-implant bone-anchored hearing devices, providers are required to submit the following:
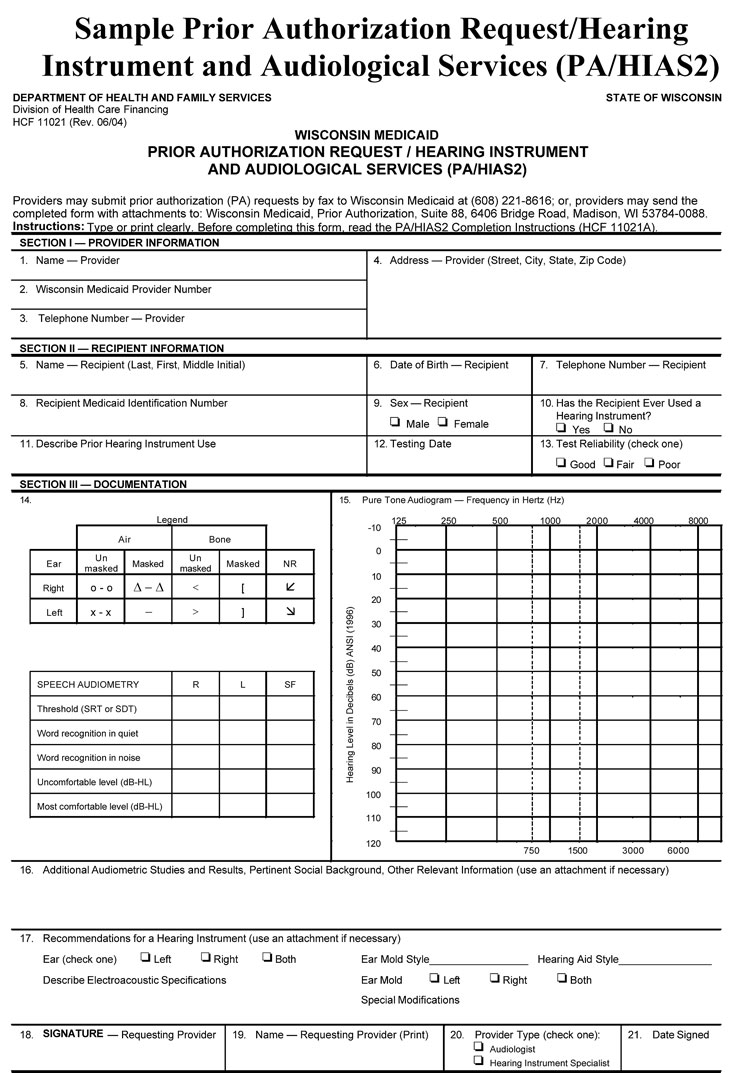
- A completed PA/HIAS1.
- A completed PA/HIAS2 documenting the medical necessity of the non-implant bone-anchored hearing device.
Topic #2985 Noncontracted Hearing Aid Models for Members Younger Than 21
Modifier TG Valid Only for Audiologists
Medicaid-enrolled audiologists may use modifier TG (Complex/high tech level of care) for members who are younger than 21 years of age.
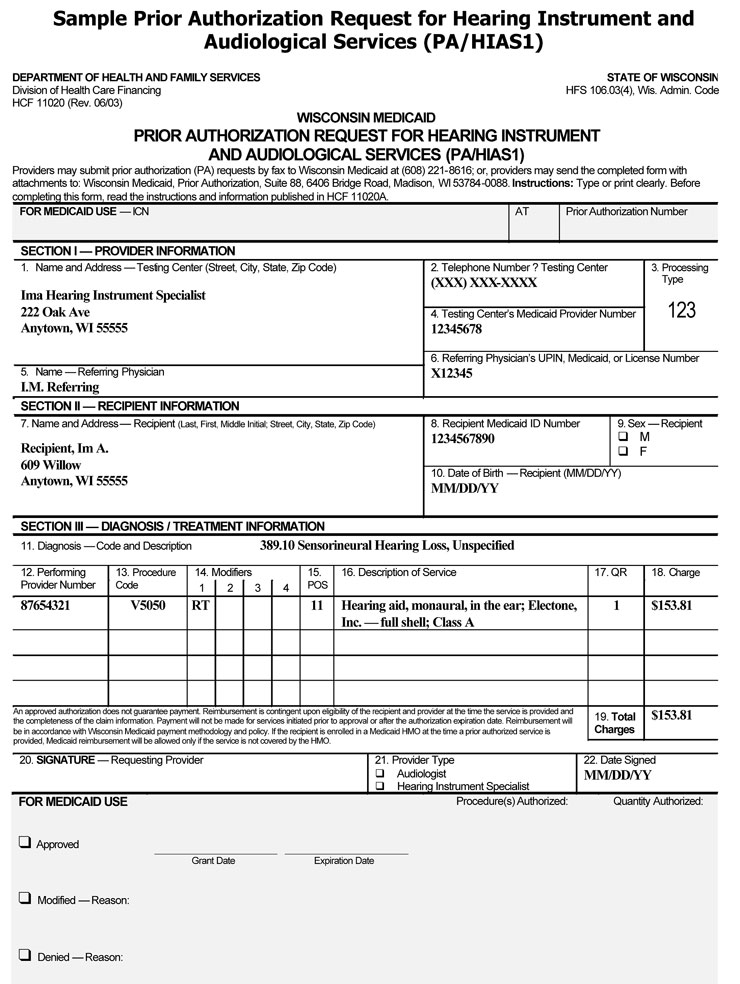
For noncontracted hearing aid models for members younger than 21 years of age, providers are required to complete the following information when requesting PA:
- A PA/HIAS1. The form must include the following:
- The most appropriate HCPCS procedure code for each requested hearing instrument.
- Modifier TG (Complex/high tech level of care).
- Modifier RT or LT, if applicable.
- The manufacturer, model number, and size (that is, full shell, half shell, low profile).
- A PA/HIAS2. The form must include the audiological needs and applicable language, educational, vocational, or physical needs of the member.
Additionally, providers are required to include the following with the PA request:
- A statement explaining why one of the hearing aid models on the ForwardHealth Hearing Aid Volume Purchase Contract will not meet the member's need.
- A copy of the manufacturer's invoice that indicates the list price charged to the audiologist. Audiologists will be reimbursed at the net cash outlay for the hearing aid. The net cash outlay for purchase is the manufacturer's invoice cost including end-of-month volume discounts.
- A copy of the manufacturer's loss and damage warranty, equipment warranty, and repair warranty.
Topic #2954 Procedure Code 92599
Providers are to use CPT code 92599 (unlisted otorhinolaryngological service or procedure) for services or procedures for which there is no specific CPT procedure code.
Procedure code 92599 should be used only when there is no other code that describes the service or procedure being offered. Only audiologists may request PA or submit claims for this code; PA requests and claims submitted by hearing instrument specialists will be denied.
PA is always required when using this code. Topic #2829 Procedure Code V5299
Use of procedure code V5299 - hearing service, miscellaneous - is limited to those instances when there is no other code to describe a specific hearing instrument or supply. PA is still required when using procedure code V5299.
Providers must include the following documentation when submitting PA requests for procedure code V5299:
- A complete description of the hearing instrument, including style, electroacoustic specifications, accessories, and the ear(s) to be fitted
- Comments addressing why the specialized hearing instrument requested with procedure code V5299 will provide measurable, significant improvement in functional hearing compared to a standard hearing instrument, a digitally programmable analog hearing instrument, or a digital hearing instrument
- Documentation verifying the cost, including a copy of manufacturer's information giving the list price
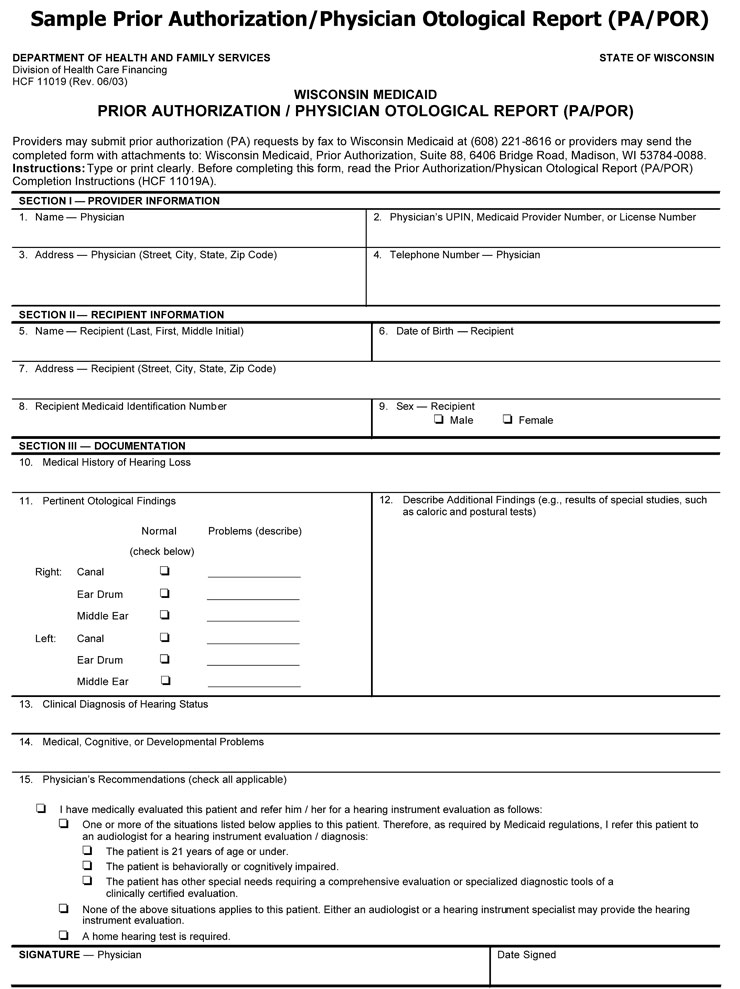
- PA/POR* is required for all PA requests by Hearing Instrument Specialists
- PA/HIAS1
- PA/HIAS2
*Hearing instrument specialists are required to use the PA/POR for all PA requests for hearing instruments and supplies. However, audiologists are not required to use the PA/POR, but must maintain a record of medical clearance for the hearing instrument in the member's file.
 |