| Program Name: | BadgerCare Plus and Medicaid | Handbook Area: | Durable Medical Equipment | | 05/18/2024 | Claims : SubmissionTopic #17797 1500 Health Insurance Claim Form Completion Instructions
These instructions are for the completion of the 1500 Health Insurance Claim Form for ForwardHealth. Refer to the
1500 Health Insurance Claim Form Reference Instruction Manual for Form Version 02/12,
prepared by the NUCC and available on their website, to view instructions for all item numbers not listed below.
Use the following claim form completion instructions, in conjunction with the 1500 Health Insurance Claim Form Reference Instruction Manual for Form Version 02/12, prepared by the NUCC, to avoid denial
or inaccurate claim payment. Be advised that every code used is required to be a valid code, even if it is entered in a non-required field. Do not include attachments unless instructed to do so.
Members enrolled in BadgerCare Plus or Medicaid receive a ForwardHealth member identification card. Always verify a member's enrollment before providing nonemergency services to determine if there are
any limitations to covered services and to obtain the correct spelling of the member's name.
When submitting a claim with multiple pages, providers are required to indicate page numbers using the format "Page X of X" in the upper right corner of the claim form.
Other health insurance sources must be billed prior to submitting claims to ForwardHealth, unless the service does not require commercial health
insurance billing as determined by ForwardHealth. When submitting paper claims, if the member has any other health insurance sources, providers are required to complete and submit an Explanation of Medical Benefits form, along with the completed paper claim.
Submit completed paper claims and the completed Explanation of Medical Benefits form, as applicable, to the following address:
ForwardHealth
Claims and Adjustments
313 Blettner Blvd
Madison WI 53784
Item Number 6 — Patient Relationship to Insured
Enter "X" in the "Self" box to indicate the member's relationship to insured when Item Number 4 is completed. Only one box can be marked.
Item Number 9 — Other Insured's Name (not required)
This field is not required on the claim.
Note: When submitting paper claims to ForwardHealth, if the member has any other health insurance sources (for example, commercial health insurance, Medicare, Medicare Advantage Plans), providers are required to complete and submit a separate Explanation of Medical Benefits form for each other payer as an attachment(s) to their completed paper claim.
Item Number 9a — Other Insured's Policy or Group Number (not required)
This field is not required on the claim.
Note: When submitting paper claims to ForwardHealth, if the member has any other health insurance sources (for example, commercial health insurance, Medicare, Medicare Advantage Plans), providers are required to complete and submit a separate Explanation of Medical Benefits form for each other payer as an attachment(s) to their completed paper claim.
Item Number 9d — Insurance Plan Name or Program Name (not required)
This field is not required on the claim.
Note: When submitting paper claims to ForwardHealth, if the member has any other health insurance sources (for example, commercial health insurance, Medicare, Medicare Advantage Plans), providers are required to complete and submit a separate Explanation of Medical Benefits form for each other payer as an attachment(s) to their completed paper claim.
Item Number 10d — Claim Codes (Designated by NUCC)
When applicable, enter the Condition Code. The Condition Codes approved for use on the 1500 Health Insurance Claim Form are available on the
NUCC website under Code Sets.
Item Number 11 — Insured's Policy Group or FECA Number (not required)
This field is not required on the claim.
Note: When submitting paper claims to ForwardHealth, if the member has any other health insurance sources (for example, commercial health insurance, Medicare, Medicare Advantage Plans), providers are required to complete and submit a separate Explanation of Medical Benefits form for each other payer as an attachment(s) to their completed paper claim.
Item Number 11d — Is There Another Health Benefit Plan?
This field is not used for processing by ForwardHealth.
Item Number 19 — Additional Claim Information (Designated by NUCC)
When applicable, enter provider identifiers or taxonomy codes. A list of applicable qualifiers are defined by the NUCC and can be found in the NUCC 1500 Health Insurance Claim Form Reference
Instruction Manual for Form Version 02/12, prepared by the NUCC.
If a provider bills an unlisted (or not otherwise classified) procedure code, a description of the
procedure must be indicated in this field. If a more specific code is not available, the provider is required to submit the appropriate documentation, which could include a PA request, to justify use of the unlisted procedure code and to describe the procedure or service rendered.
Item Number 22 — Resubmission Code and/or Original Reference Number
This field is not used for processing by ForwardHealth.
Section 24
The six service lines in section 24 have been divided horizontally. Enter service information in the bottom, unshaded area of the six service lines. The horizontal division of each service line is not
intended to allow the billing of 12 lines of service.
For physician-administered drugs: NDCs must be indicated in the shaded area of Item Numbers 24A-24G. Each NDC must be accompanied by an NDC qualifier, unit
qualifier, and units. To indicate an NDC, providers should do the following:
- Indicate the NDC qualifier N4, followed by the 11-digit NDC, with no space in between
- Indicate one space between the NDC and the unit qualifier
- Indicate one unit qualifier (F2 [International unit], GR [Gram], ME [Milligram], ML [Milliliter], or UN [Unit]), followed by the NDC units, with no space in between
For additional information about submitting a 1500 Health Insurance Claim Form with supplemental NDC information, refer to the completion instructions located under "Section 24" in the Field Specific
Instructions section of the NUCC's 1500 Health Insurance Claim Form Reference Instruction Manual for Form Version 02/12.
Item Number 24C — EMG
Enter a "Y" in the unshaded area for each procedure performed as an emergency. If the procedure was not an emergency, leave this field blank.
Item Number 29 — Amount Paid (not required)
This field is not required on the claim.
Note: When submitting paper claims to ForwardHealth, if the member has any other health insurance sources (for example, commercial health insurance, Medicare, Medicare Advantage Plans), providers are required to complete and submit a separate Explanation of Medical Benefits form for each other payer as an attachment(s) to their completed paper claim. Topic #542 Attached Documentation
Providers should not submit additional documentation with a claim unless specifically requested. Topic #19677 Bone-Anchored Hearing Devices and Cochlear Implants
Wisconsin Medicaid separately reimburses DME providers for bone-anchored hearing devices and cochlear implants when the implant surgery is performed in an ASC or outpatient hospital and the rendering surgeon has submitted a claim for the surgery. The POS codes for these facilities are as follows:
- "11" (Office)
- "19" (Off Campus — Outpatient Hospital)
- "22" (On Campus — Outpatient Hospital)
- "24" (Ambulatory Surgical Center)
Claims for bone-anchored hearing devices and bone-anchored hearing device surgery and cochlear implants and cochlear implant surgery are required to be submitted in a professional claim format (e.g., electronically using and 837 transaction, Direct Data Entry on the Portal, or Provider Electronic Solutions claims submission software, or on paper using the 1500 Health Insurance Claim Form).
The rendering surgeon is required to submit the claim for the surgery; the DME provider is required to submit the claim for the device.
Note: ForwardHealth will confirm that a claim for the bone-anchored hearing device surgery or cochlear implant surgery has been submitted prior to processing the DME provider's claim for the device. The DME provider is required to coordinate with the surgeon to ensure that the surgical claim is submitted first. Topic #15737 Claims for Services Prescribed, Referred, or Ordered
Claims for services that are prescribed, referred, or ordered must include the NPI of the Medicaid-enrolled provider who prescribed, referred, or ordered the service. Claims that do not include the NPI of a Medicaid-enrolled provider will be denied. (However, providers should not include the NPI of a provider who prescribes, refers, or orders services on claims for services that are not prescribed, referred, or ordered, as those claims will also deny if the provider is not Medicaid-enrolled.)
Note: Claims submitted for ESRD services do not require referring provider information; however, prescribing and ordering provider information will still be required on claims.
Contacting Prescribing/Referring/Ordering Provider After a Claim Denial
If a claim for services prescribed, referred, or ordered is denied because the prescribing/referring/ordering provider was not Medicaid-enrolled, the rendering provider should contact the prescribing/referring/ordering provider and do the following:
- Communicate that the prescribing/referring/ordering provider is required to be Medicaid-enrolled
- Inform the prescribing/referring/ordering provider of the limited enrollment available for prescribing/referring/ordering providers
- Resubmit the claim once the prescribing/referring/ordering provider has enrolled in Wisconsin Medicaid
Exception for Services Prescribed, Referred, or Ordered Prior to a Member's Medicaid Enrollment
Providers may submit claims for services prescribed, referred, or ordered by a non-Medicaid-enrolled provider if the member was not yet enrolled in Wisconsin Medicaid at the time the prescription, referral, or order was written (and the member has since enrolled in Wisconsin Medicaid). However, once the prescription, referral, or order expires, the prescribing/referring/ordering provider is required to enroll in Wisconsin Medicaid if they continue to prescribe, refer, or order services for the member.
The procedures for submitting claims for this exception depend on the type of claim submitted:
- Institutional, professional, and dental claims for this exception must be sent to the following address:
ForwardHealth
P.R.O. Exception Requests
Ste 50
313 Blettner Blvd
Madison WI 53784
A copy of the prescription, referral, or order must be included with the claim.
- Pharmacy and compound claims for this exception do not require any special handling. These claims include a prescription date, so they can be processed to bypass the prescriber Medicaid enrollment requirement in situations where the provider prescribed services before the member was Medicaid-enrolled.
Topic #6957 Copy Claims on the ForwardHealth Portal
Providers can copy institutional, professional, and dental paid claims on the ForwardHealth Portal. Providers can open any paid claim, click the "Copy" button, and all of the information on the claim will be copied over to a new claim form. Providers can then make any desired changes to the claim form and click "Submit" to submit as a new claim. After submission, ForwardHealth will issue a response with a new ICN along with the claim status. Topic #5017 Correct Errors on Claims and Resubmit to ForwardHealth on the Portal
Providers can view EOB codes and descriptions for any claim submitted to ForwardHealth on the ForwardHealth Portal. The EOBs help providers determine why a claim did not process successfully, so providers may correct the error online and resubmit the claim. The EOB appears on the bottom of the screen and references the applicable claim header or detail. Topic #10137 Compound and Noncompound Drug Claims
For example, the provider might see on his or her RA the detail for a noncompound drug claim was denied with the EOB code indicating that the detail on the claim was not processed due to an error. The provider may then correct the error on the claim via the Portal online screen application and resubmit the claim to ForwardHealth. Topic #1729 Dates of Service
ForwardHealth defines the DOS as follows:
- The date on which the DME was dispensed to the member or the member's caregiver by the provider
- The date on which the DME was shipped or mailed to the member or the member's caregiver if the provider used a shipping service or mail order
Rental items billed to ForwardHealth must have "from" and "to" DOS. If the item was provided on consecutive days, those dates may be indicated as a range of dates by entering the first date as the "from" DOS and the last date as the "to" DOS. The number of days indicated must equal the number of days within the range. Rental items must be ranged within the same calendar month per detail line.
The "to" DOS requirement does not apply to Medicare crossover claims.
For purchased items, indicate only one specific DOS for each purchase, not a range of dates. A range of two consecutive dates is acceptable, such as May 4, 2008, to May 5, 2008. Topic #4997 Direct Data Entry of Professional and Institutional Claims on the Portal
Providers can submit the following claims to ForwardHealth via DDE on the ForwardHealth Portal:
- Professional claims
- Institutional claims
- Dental claims
- Compound drug claims
- Noncompound drug claims
DDE is an online application that allows providers to submit claims directly to ForwardHealth.
When submitting claims via DDE, required fields are indicated with an asterisk next to the field. If a required field is left blank, the claim will not be submitted and a message will appear prompting the provider to complete the specific required field(s). Portal help is available for each online application screen. In addition, search functions accompany certain fields so providers do not need to look up the following information in secondary resources.
On professional claim forms, providers may search for and select the following:
- Procedure codes
- Modifiers
- Diagnosis codes
- Place of service codes
On institutional claim forms, providers may search for and select the following:
- Type of bill
- Patient status
- Visit point of origin
- Visit priority
- Diagnosis codes
- Revenue codes
- Procedure codes
- HIPPS codes
- Modifiers
On dental claims, providers may search for and select the following:
- Procedure codes
- Rendering providers
- Area of the oral cavity
- Place of service codes
On compound and noncompound drug claims, providers may search for and select the following:
- Diagnosis codes
- NDCs
- Place of service codes
- Professional service codes
- Reason for service codes
- Result of service codes
Using DDE, providers may submit claims for compound drugs and single-entity drugs. Any provider, including a provider of DME or of DMS who submits noncompound drug claims, may submit these claims via DDE. All claims, including POS claims, are viewable via DDE. Topic #344 Electronic Claim Submission
Providers are encouraged to submit claims electronically. Electronic claim submission does the following:
- Adapts to existing systems
- Allows flexible submission methods
- Improves cash flow
- Offers efficient and timely payments
- Reduces billing and processing errors
- Reduces clerical effort
Topic #2045 Electronic Claim Submission for Durable Medical Equipment
Electronic claims for DME must be submitted using the 837P transaction. Electronic claims for DME submitted using any transaction other than the 837P will be denied.
Providers should use the companion guide for the 837P transaction when submitting these claims.
Provider Electronic Solutions Software
The DMS offers electronic billing software at no cost to providers. The PES software allows providers to submit electronic claims using an 837 transaction. To obtain PES software, providers may download it from the ForwardHealth Portal. For assistance installing and using PES software, providers may call the EDI Helpdesk. Topic #2333 Point-of-Sale Claims
BadgerCare Plus, Medicaid, and SeniorCare use a voluntary pharmacy POS electronic claims management system. The POS system enables providers to submit electronic pharmacy claims for legend and OTC drugs in an online, real-time environment.
The pharmacy system verifies member enrollment and monitors pharmacy policy. Within seconds of submitting a real-time claim, these processes are completed and the provider receives an electronic response indicating payment or denial.
National Council for Prescription Drug Programs D.0 Telecommunications Standard Claims
BadgerCare Plus, Medicaid, and SeniorCare use the NCPDP Telecommunication Standard Format Version D.0. Using this format, providers are able to complete the following:
- Initiate new claims and reverse and resubmit previously paid real-time claims
- Submit individual claims or a batch of claims for the same member within one electronic transmission
- Submit claims for compound drugs
Cardholder ID
If the member identification number submitted on a claim is not the most current member ID on file with ForwardHealth, the claim will be denied and the Cardholder ID (302-C2) field on the claim response will include the current member ID.
Other Amount Claimed Submitted
Wisconsin Medicaid does not reimburse for charges (i.e., postage, shipping, administrative costs) indicated in the Other Amount Claimed Submitted (480-H9) field. Claims will be denied if a provider indicates a charge in the Other Amount Claimed Submitted field.
National Provider Identifier On Compound and Noncompound Claims
Billing Providers
An NPI is required on compound and noncompound claims. Providers who do not have a unique NPI for each enrollment are required to select one Medicaid enrollment as the "default" enrollment. Claims will be processed using the provider file information from the default enrollment.
Prescriber ID and Prescriber ID Qualifier
An NPI is the only identifier accepted on compound and noncompound claims, including paper claims. Billing providers are required to make every effort possible to obtain the prescribing provider's NPI. Only in instances when the billing provider is unable to obtain the prescriber's NPI may the billing provider indicate their own NPI in the Prescriber ID field. DEA numbers, including "default" DEA numbers, are not accepted for the Prescriber ID on pharmacy claims.
Direct Data Entry of Claims on the Portal
Claims for compound drugs and noncompound drugs may be submitted to ForwardHealth using DDE on the ForwardHealth Portal. DDE is an online application that allows providers to submit claims directly to ForwardHealth.
When submitting claims via DDE, required fields are indicated with an asterisk next to the field. If a required field is left blank, the claim will not be submitted and a message will appear, prompting the provider to complete the specific required field(s). Portal help is available for each online application screen. In addition, search functions accompany certain fields so providers do not need to look up the following information in secondary resources.
On compound and noncompound drug claims, providers may search for and select the following:
- Diagnosis codes
- NDCs
- Place of service codes
- Professional service codes
- Reason for service codes
- Result of service codes
Using DDE, providers may submit claims for compound drugs and single-entity drugs. Any provider, including a provider of DME or of DMS who submits noncompound drug claims, may submit these claims via DDE. All claims, including POS claims, are viewable via DDE.
Provider Electronic Solutions Software
ForwardHealth offers electronic billing software at no cost to providers. PES software allows providers to submit NCPDP 1.1 batch format pharmacy transactions, reverse claims, and check claim status. To obtain PES software, providers may download it from the ForwardHealth Portal. For assistance installing and using PES software, providers may call the EDI Helpdesk. Topic #16937 Electronic Claims and Claim Adjustments With Other Commercial Health Insurance Information
Effective for claims and claim adjustments submitted electronically via the Portal or PES software on and after June 16, 2014, other insurance information must be submitted at the detail level on professional, institutional, and dental claims and adjustments if it was processed at the detail level by the primary insurance. Except for a few instances, Wisconsin Medicaid or BadgerCare Plus is the payer of last resort for any covered services; therefore, providers are required to make a reasonable effort to exhaust all existing other health insurance sources before submitting claims to ForwardHealth or to a state-contracted MCO.
Other insurance information that is submitted at the detail level via the Portal or PES software will be processed at the detail level by ForwardHealth.
Under HIPAA, claims and adjustments submitted using an 837 transaction must include detail-level information for other insurance if they were processed at the detail level by the primary insurance.
Adjustments to Claims Submitted Prior to June 16, 2014
Providers who submit professional, institutional, or dental claim adjustments electronically on and after June 16, 2014, for claims originally submitted prior to June 16, 2014, are required to submit other insurance information at the detail level on the adjustment if it was processed at the detail level by the primary insurance. Topic #365 Extraordinary Claims
Extraordinary claims are claims that have been denied by a BadgerCare Plus HMO or SSI HMO and should be submitted to fee-for-service. Topic #4837 HIPAA-Compliant Data Requirements
Procedure Codes
All fields submitted on paper and electronic claims are edited to ensure HIPAA compliance before being processed. Compliant code sets include CPT and HCPCS procedure codes entered into all fields, including those fields that are "Not Required" or "Optional."
If the information in all fields is not valid and recognized by ForwardHealth, the claim will be denied.
Provider Numbers
For health care providers, NPIs are required in all provider number fields on paper claims and 837 transactions, including rendering, billing, referring, prescribing, attending, and "Other" provider fields.
Non-healthcare providers, including personal care providers, SMV providers, blood banks, and CCOs should enter valid provider numbers into fields that require a provider number. Topic #20057 Home Ventilator Rental
When submitting claims for primary and back-up or secondary home ventilator rental, providers are required to indicate one of the following allowable HCPCS procedure codes, as applicable:
- E0465 (Home ventilator; any type, used with invasive interface, [e.g., tracheostomy tube])
- E0466 (Home ventilator; any type, used with non-invasive interface, [e.g., mask, chest shell])
Note: Due to advances in technology, some devices have multiple capabilities, including functioning as a BiPap, C-Pap, or RAD. These devices should not be submitted on a claim using the above procedure codes for a home ventilator.
Modifiers
Providers are required to include the following modifiers, as appropriate on claims and PA requests for primary and back-up or secondary home ventilator rental:
- RR (Rental)
- TW (Back-up or secondary home ventilator)
Unit Measure
One unit represents one calendar month of rental. Providers are required to indicate a unit of 1 on claims and PA requests to represent one calendar month of rental.
Date of Service
Providers should only indicate a single DOS on claims for primary and back-up or secondary home ventilator rental. The DOS can be any one date within the calendar month. Claims with span billing will be denied. Topic #562 Managed Care Organizations
Claims for services that are covered in a member's state-contracted MCO should be submitted to that MCO. Topic #10837 Note Field for Most Claims Submitted Electronically
In some instances, ForwardHealth requires providers to include a description of a service identified by an unlisted, or NOC, procedure code. Providers submitting claims electronically should include a description of an NOC procedure code in a "Notes" field, if required. The Notes field allows providers to enter up to 80 characters. In some cases, the Notes field allows providers to submit NOC procedure code information on a claim electronically instead of on a paper claim or with a paper attachment to an electronic claim.
The Notes field should only be used for NOC procedure codes that do not require PA.
Claims Submitted via the ForwardHealth Portal Direct Data Entry or Provider Electronic Solutions
A notes field is available on the ForwardHealth Portal DDE and PES software when providers submit the following types of claims:
- Professional
- Institutional
- Dental
On the professional form, the Notes field is available on each detail. On the institutional and dental forms, the Notes field is only available on the header.
Claims Submitted via 837 Health Care Claim Transactions
ForwardHealth accepts and utilizes information submitted by providers about NOC procedure codes in certain loops/segments on the 837 transactions. Refer to the companion guides for more information. Topic #17757 Providers are reminded to submit claims for services with the most accurate procedure codes for all services and equipment. The
DME Index includes allowable procedure codes, associated maximum allowable fees, and POS information.
Diabetic Shoes or Inserts
When submitting claims for diabetic shoes or inserts, providers are required to do the following:
- Record each procedure code representing the shoe or unit as a separate line item. Refer to the specific procedure code description to determine the number of units.
- Indicate the RT (right side) or LT (left side) modifier, as appropriate, on separate line items of the claim.
Orthopedic or Corrective Shoes and Foot Orthotics
When submitting claims for orthopedic or corrective shoes and foot orthotics, providers are required to record each procedure code representing the shoe or unit as a separate line item. Refer to the specific procedure code description to determine the number of units:
- If code description indicates "each," indicate the RT (right side) or LT (left side) modifier, as appropriate, on separate line items of the claim or PA request.
- If the code description indicates "pair," indicate no modifier. Submit as one line item as a unit of one on the claim or PA request.
Topic #561 Paper Claim Form Preparation and Data Alignment Requirements
Optical Character Recognition
Paper claims submitted to ForwardHealth on the 1500 Health Insurance Claim Form and UB-04 Claim Form are processed using OCR software that recognizes printed, alphanumeric text. OCR software increases efficiency by alleviating the need for keying in data from paper claims.
The data alignment requirements do not apply to the Compound Drug Claim form and the Noncompound Drug Claim form.
Speed and Accuracy of Claims Processing
OCR software processes claim forms by reading text within fields on claim forms. After a paper claim form is received by ForwardHealth, the claim form is scanned so that an image can be displayed
electronically. The OCR software reads the electronic image on file and populates the information into the ForwardHealth interChange system. This technology increases accuracy by removing the possibility of errors being made during manual keying.
OCR software speeds paper claim processing, but only if providers prepare their claim forms correctly. In order for OCR software to read the claim form accurately, the quality of copy and the alignment of text within individual fields on the claim form need to be precise. If data are misaligned, the claim could be processed incorrectly. If data cannot be read by the OCR software, the process will stop and the electronic image of the claim form will need to be reviewed and keyed manually. This will cause an increase in processing time.
Handwritten Claims
Submitting handwritten claims should be avoided whenever possible. ForwardHealth accepts handwritten claims; however, it is very difficult for OCR software to read a handwritten claim. If a handwritten claim cannot be read by the OCR software, it will need to be keyed manually from the electronic image of the claim form. Providers should avoid submitting claims
with handwritten corrections as this can also cause OCR software processing delays.
Use Original Claim Forms
Only original 1500 Health Insurance Claim Forms and UB-04 Claim Forms should
be submitted. Original claim forms are printed in red ink and may be obtained
from a federal forms supplier. ForwardHealth does not provide these claim forms.
Claims that are submitted as photocopies cannot be read by OCR software and will
need to be keyed manually from an electronic image of the claim form. This could
result in processing delays.
Use Laser or Ink Jet Printers
It is recommended that claims are printed using laser or ink jet printers
rather than printers that use DOT matrix. DOT matrix printers have breaks in the
letters and numbers, which may cause the OCR software to misread the claim form.
Use of old or worn ink cartridges should also be avoided. If the claim form is
read incorrectly by the OCR software, the claim may be denied or reimbursed
incorrectly. The process may also be stopped if it is unable to read the claim
form, which will cause a delay while it is manually reviewed.
Alignment
Alignment within each field on the claim form needs to be accurate. If text
within a field is aligned incorrectly, the OCR software may not recognize that
data are present within the field or may not read the data correctly. For
example, if a reimbursement amount of $300.00 is entered into a field on the
claim form, but the last "0" is not aligned within the field, the OCR software
may read the number as $30.00, and the claim will be reimbursed incorrectly.
To get the best alignment on the claim form, providers should center
information vertically within each field, and align all information on the same
horizontal plane. Avoid squeezing two lines of text into one of the six line
items on the 1500 Health Insurance Claim Form.
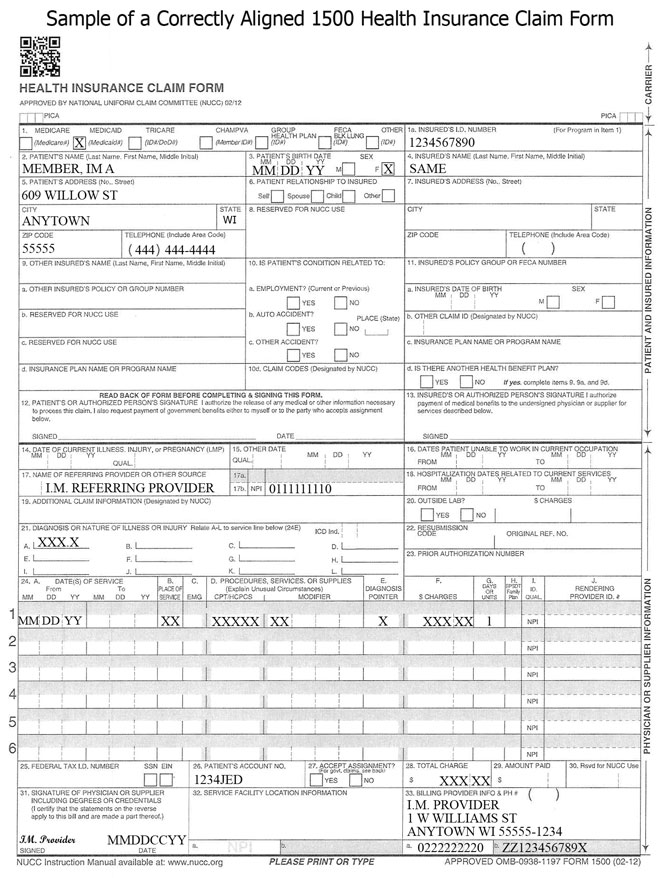
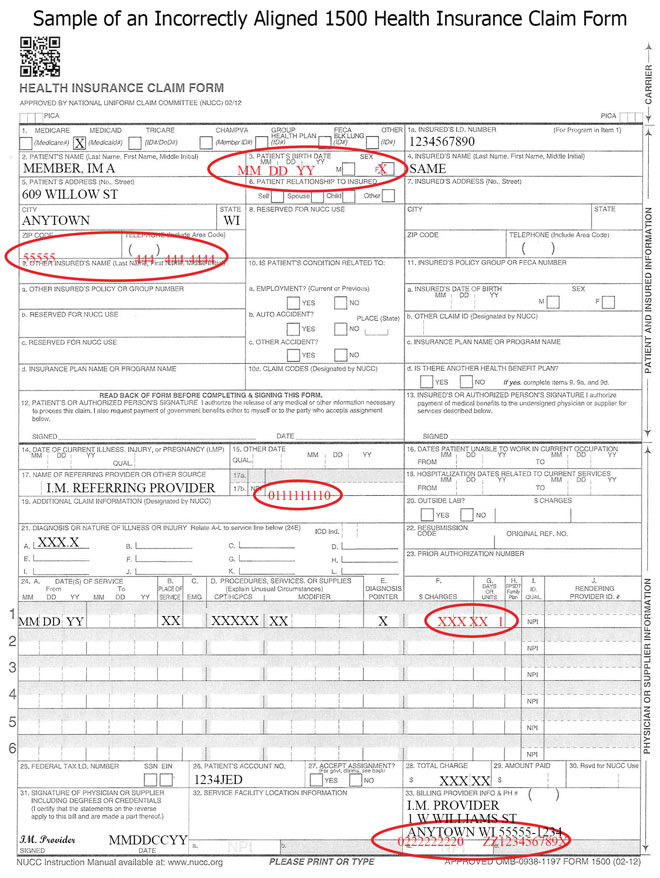
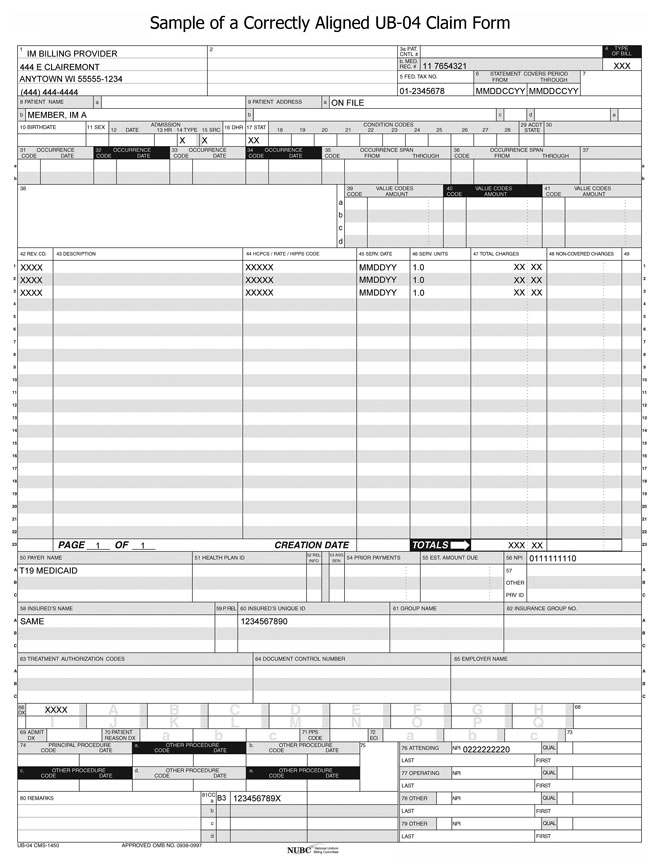
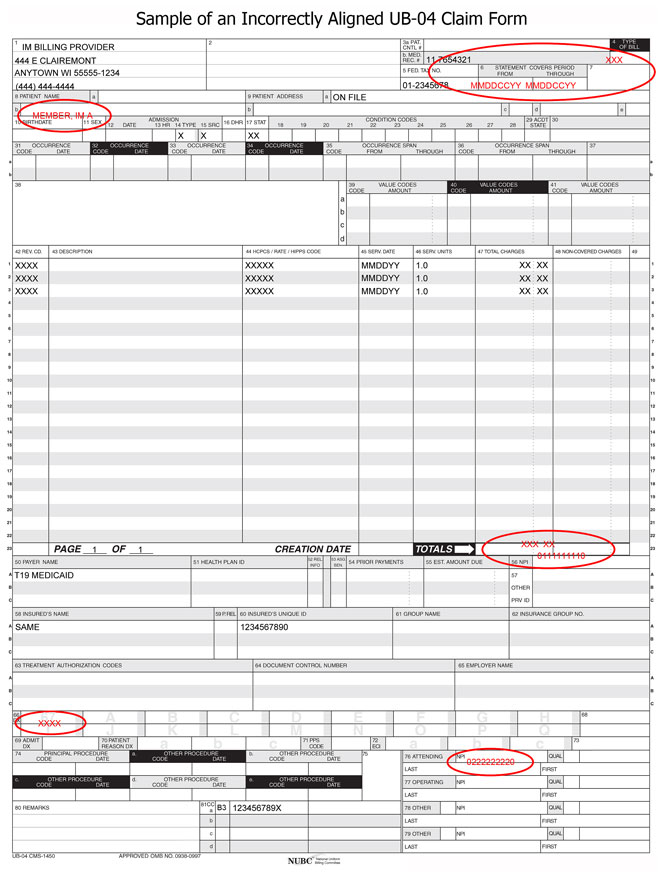
The following sample claim forms demonstrate correct and incorrect alignment:
Clarity
Clarity is very important. If information on the claim form is not clear
enough to be read by the OCR software, the process may stop, prompting manual
review.
The following guidelines will produce the clearest image and optimize
processing time:
- Use 10-point or 12-point Times New Roman or Courier New font.
- Type all claim data in uppercase letters.
- Use only black ink to complete the claim form.
- Avoid using italics, bold, or script.
- Make sure characters do not touch.
- Make sure there are no lines from the printer cartridge anywhere on the
claim form.
- Avoid using special characters such as dollar signs, decimals, dashes,
asterisks, or backslashes, unless it is specified that these characters should
be used.
- Use Xs in check boxes. Avoid using letters such as "Y" for "Yes," "N" for
"No," "M" for "Male," or "F" for "Female."
- Do not highlight any information on the claim form. Highlighted
information blackens when it is imaged, and the OCR software will be unable to
read it.
Note: The above guidelines will also produce the clearest image for
claims that need to be keyed manually from an electronic image.
Staples, Correction Liquid, and Correction Tape
The use of staples, correction liquid, correction tape, labels, or stickers
on claim forms should be avoided. Staples need to be removed from claim forms
before they can be imaged, which can damage the claim and cause a delay in
processing time. Correction liquid, correction tape, labels, and stickers can
cause data to be read incorrectly or cause the OCR process to stop, prompting
manual review. If the form cannot be read by the OCR software, it will need to
be keyed manually from an electronic image.
Additional Diagnosis Codes
ForwardHealth will accept up to 12 diagnosis codes in Item Number 21 of the
1500 Health Insurance Claim Form.
 Topic #2046 Paper Claim Submission
Paper claims for DME, except for diabetic supplies, must be submitted using the 1500 Health Insurance Claim Form.
Providers should use the appropriate claim form instructions for DME when submitting these claims.
Obtaining the Claim Forms
ForwardHealth does not provide the 1500 Health Insurance Claim Form. The form may be obtained from any federal forms supplier. Topic #9117 Paper Claim Submission for Diabetic Supplies
Paper claims for diabetic supplies must be submitted on a Noncompound Drug Claim form with two exceptions:
- There is an approved PA on file.
- The claim is a Medicare Part B crossover claim.
Submit completed paper claim forms for payment to the following address:
ForwardHealth
313 Blettner Blvd
Madison WI 53784
To order paper claim forms, providers may call Provider Services, or write to the following address:
ForwardHealth
Form Reorder
313 Blettner Blvd
Madison, WI 53784
Providers should indicate the number of forms needed in their written request. Topic #22797 Payment Integrity Review Supporting Documentation
Providers are notified that an individual claim is subject to PIR through a message on the Portal when submitting claims. When this occurs, providers have seven calendar days to submit the supporting documentation that must be retained in the member's record for the specific service billed. This documentation must be attached to the claim. The following are examples of documentation providers may attach to the claim; however, this list is not exhaustive, and providers may submit any documentation available to substantiate payment:
- Case management or consultation notes
- Durable medical equipment or supply delivery receipts or proof of delivery and itemized invoices or bills
- Face-to-face encounter documentation
- Individualized plans of care and updates
- Initial or program assessments and questionnaires to indicate the start DOS
- Office visit documentation
- Operative reports
- Prescriptions or test orders
- Session or service notice for each DOS
- Testing and lab results
- Transportation logs
- Treatment notes
Providers must attach this documentation to the claim at the time of, or up to seven days following, submission of the claim. A claim may be denied if the supporting documentation is not submitted. If a claim is denied, providers may submit a new claim with the required documentation for reconsideration. To reduce provider impact, claims reviewed by the OIG will be processed as quickly as possible, with an expected average adjudication of 30 days. Topic #10177 Prior Authorization Numbers on Claims
Providers are not required to indicate a PA number on claims. ForwardHealth interChange matches the claim with the appropriate approved PA request. ForwardHealth's RA and the 835 report to the provider the PA number used to process a claim. If a PA number is indicated on a claim, it will not be used and it will have no effect on processing the claim.
When a PA requirement is added to the list of drugs requiring PA and the effective date of a PA falls in the middle of a billing period, two separate claims that coincide with the presence of PA for the drug must be submitted to ForwardHealth. Topic #3868 Referring Providers
Claims for DME require the referring provider's name and NPI. Topic #10637 Reimbursement Reduction for Most Paper Claims
As a result of the Medicaid Rate Reform project, ForwardHealth will reduce reimbursement on most claims submitted to ForwardHealth on paper. Most paper claims will be subject up to a $1.10 reimbursement reduction per claim.
For each claim that a reimbursement reduction was applied, providers will receive an EOB to notify them of the payment reduction. For claims with reimbursement reductions, the EOB will state the following, "This claim is eligible for electronic submission. Up to a $1.10 reduction has been applied to this claim payment."
If a paid claim's total reimbursement amount is less than $1.10, ForwardHealth will reduce the payment up to a $1.10. The claim will show on the RA as paid but with a $0 paid amount.
The reimbursement reduction applies to the following paper claims:
Exceptions to Paper Claim Reimbursement Reduction
The reimbursement reduction will not affect the following providers or claims:
- In-state emergency providers
- Out-of-state providers
- Medicare crossover claims
- Any claims that ForwardHealth requires additional supporting information to be submitted on paper, such as:
Topic #3504 Requirements for Compression Garments
In this topic, the term "compression garments" is used to refer to both gradient compression garments and compression burn garments, unless otherwise stated.
The following table contains information required on claims submissions for compression garments.
| Procedure Code |
Claim
Attachment?1 |
RT and/or LT Modifier Required? |
Reorder (RA) Modifier?2 |
Allowable ICD Diagnosis Codes Without Prior Authorization3 |
| A6501 |
Yes |
No |
Yes |
T30.0, T30.4 |
| A6502 |
No |
No |
Yes |
T20.00XA*–T20.79XS* (Excluding codes with "9" as the sixth character), T26.21XA*–T26.22XS*, T26.41XA*–T26.42XS* |
| A6503 |
No |
No |
Yes |
T20.00XA*–T20.79XS* (Excluding codes with "9" as the sixth character), T26.21XA*–T26.22XS*, T26.41XA*–T26.42XS*, T26.51XA*–T26.52XS* |
| A6504 |
No |
Yes |
Yes |
T23.001A*–T23.792S* (Excluding codes with "9" as the sixth character) |
| A6505 |
No |
Yes |
Yes |
T22.00XA*–T22.092S* (Excluding codes with "9" as the sixth character), T22.111A*–T22.192S* (Excluding codes with "9" as the sixth character), T22.211A*–T22.493S* (Excluding codes with "9" as the sixth character), T22.511A*–T22.592S* (Excluding codes with "9" as the sixth character), T22.611A*–T23.792S* (Excluding codes with "9" as the sixth character) |
| A6506 |
No |
Yes |
Yes |
T22.00XA*–T22.092S* (Excluding codes with "9" as the sixth character), T22.111A*–T22.192S* (Excluding codes with "9" as the sixth character), T22.211A*–T22.493S* (Excluding codes with "9" as the sixth character), T22.511A*–T22.592S* (Excluding codes with "9" as the sixth character), T22.611A*–T23.792S* (Excluding codes with "9" as the sixth character) |
| A6507 |
No |
Yes |
Yes |
T24.001A*–T25.792S* (Excluding codes with "9" as the sixth character) |
| A6508 |
No |
Yes |
Yes |
T24.001A*–T25.792S* (Excluding codes with "9" as the sixth character) |
| A6509 |
No |
No |
Yes |
T21.00XA*–T21.79XS* |
| A6510 |
No |
No |
Yes |
T21.00XA*–T22.099S*, T22.10XA*–T22.392S* (Excluding codes with "9" as the sixth character), T22.40XA*–T22.499S*, T22.50XA*–T22.792S* (Excluding codes with "9" as the sixth character) |
| A6511 |
No |
No |
Yes |
T21.30XA*–T21.39XS*, T21.70XA*–T21.79XS* |
| A6512 |
Yes |
No |
Yes |
T30.0, T30.4 |
| A6513 |
No |
No |
Yes |
T20.00XA*–T20.79XS* (Excluding codes with "9" as the sixth character), T26.01XA*–T26.02XS*, T26.21XA*–T26.22XS*, T26.41XA*–T26.42XS*, T26.51XA*–T26.52XS* |
| A6530 |
No |
Yes |
No |
I70.231–I70.249, I70.331–I70.349, I70.431–I70.449, I70.531–I70.549, I70.631–I70.649, I70.731–I70.749,
I83.011–I83.029, I83.11–I83.12, I83.211–I83.813, I83.891–I83.893, I83.91–I83.93, I87.001–I87.093 (Excluding codes with "9" as the sixth character), I87.2, I89.0, L97.111–L97.129, L97.211–L97.229, L97.311–L97.329, L97.411–L97.429, L97.511–L97.529, L97.811–L97.829, L97.911–L97.929, O12.00, O12.04, O12.05, O12.20, O12.24. O12.25, O26.00, Q82.0 |
| A6531 |
No |
Yes |
No |
I70.231–I70.249, I70.331–I70.349, I70.431–I70.449, I70.531–I70.549, I70.631–I70.649, I70.731–I70.749,
I83.011–I83.029, I83.11–I83.12, I83.211–I83.813, I83.891–I83.893, I83.91–I83.93, I87.001–I87.093 (Excluding codes with "9" as the sixth character), I87.2, I89.0, L97.111–L97.129, L97.211–L97.229, L97.311–L97.329, L97.411–L97.429, L97.511–L97.529, L97.811–L97.829, L97.911–L97.929, O12.00, O12.04, O12.05, O12.20, O12.24. O12.25, O26.00, Q82.0 |
| A6532 |
No |
Yes |
No |
I70.231–I70.249, I70.331–I70.349, I70.431–I70.449, I70.531–I70.549, I70.631–I70.649, I70.731–I70.749,
I83.011–I83.029, I83.11–I83.12, I83.211–I83.813, I83.891–I83.893, I83.91–I83.93, I87.001–I87.093 (Excluding codes with "9" as the sixth character), I87.2, I89.0, L97.111–L97.129, L97.211–L97.229, L97.311–L97.329, L97.411–L97.429, L97.511–L97.529, L97.811–L97.829, L97.911–L97.929, O12.00, O12.04, O12.05, O12.20, O12.24. O12.25, O26.00, Q82.0 |
| A6533 |
No |
Yes |
No |
I70.231–I70.249, I70.331–I70.349, I70.431–I70.449, I70.531–I70.549, I70.631–I70.649, I70.731–I70.749,
I83.011–I83.029, I83.11–I83.12, I83.211–I83.813, I83.891–I83.893, I83.91–I83.93, I87.001–I87.093 (Excluding codes with "9" as the sixth character), I87.2, I89.0, L97.111–L97.129, L97.211–L97.229, L97.311–L97.329, L97.411–L97.429, L97.511–L97.529, L97.811–L97.829, L97.911–L97.929, O12.00, O12.04, O12.05, O12.20, O12.24. O12.25, O26.00, Q82.0 |
| A6534 |
No |
Yes |
No |
I70.231–I70.249, I70.331–I70.349, I70.431–I70.449, I70.531–I70.549, I70.631–I70.649, I70.731–I70.749,
I83.011–I83.029, I83.11–I83.12, I83.211–I83.813, I83.891–I83.893, I83.91–I83.93, I87.001–I87.093 (Excluding codes with "9" as the sixth character), I87.2, I89.0, L97.111–L97.129, L97.211–L97.229, L97.311–L97.329, L97.411–L97.429, L97.511–L97.529, L97.811–L97.829, L97.911–L97.929, O12.00, O12.04, O12.05, O12.20, O12.24, O12.25, O26.00, Q82.0 |
| A6535 |
No |
Yes |
No |
I70.231–I70.249, I70.331–I70.349, I70.431–I70.449, I70.531–I70.549, I70.631–I70.649, I70.731–I70.749,
I83.011–I83.029, I83.11–I83.12, I83.211–I83.813, I83.891–I83.893, I83.91–I83.93, I87.001–I87.093 (Excluding codes with "9" as the sixth character), I87.2, I89.0, L97.111–L97.129, L97.211–L97.229, L97.311–L97.329, L97.411–L97.429, L97.511–L97.529, L97.811–L97.829, L97.911–L97.929, O12.00, O12.04, O12.05, O12.20, O12.24, O12.25, O26.00, Q82.0 |
| A6536 |
No |
Yes |
No |
I70.231–I70.249, I70.331–I70.349, I70.431–I70.449, I70.531–I70.549, I70.631–I70.649, I70.731–I70.749,
I83.011–I83.029, I83.11–I83.12, I83.211–I83.813, I83.891–I83.893, I83.91–I83.93, I87.001–I87.093 (Excluding codes with "9" as the sixth character), I87.2, I89.0, L97.111–L97.129, L97.211–L97.229, L97.311–L97.329, L97.411–L97.429, L97.511–L97.529, L97.811–L97.829, L97.911–L97.929, O12.00, O12.04, O12.05, O12.20, O12.24, O12.25, O26.00, Q82.0 |
| A6537 |
No |
Yes |
No |
I70.231–I70.249, I70.331–I70.349, I70.431–I70.449, I70.531–I70.549, I70.631–I70.649, I70.731–I70.749,
I83.011–I83.029, I83.11–I83.12, I83.211–I83.813, I83.891–I83.893, I83.91–I83.93, I87.001–I87.093 (Excluding codes with "9" as the sixth character), I87.2, I89.0, L97.111–L97.129, L97.211–L97.229, L97.311–L97.329, L97.411–L97.429, L97.511–L97.529, L97.811–L97.829, L97.911–L97.929, O12.00, O12.04, O12.05, O12.20, O12.24, O12.25, O26.00, Q82.0 |
| A6538 |
No |
Yes |
No |
I70.231–I70.249, I70.331–I70.349, I70.431–I70.449, I70.531–I70.549, I70.631–I70.649, I70.731–I70.749,
I83.011–I83.029, I83.11–I83.12, I83.211–I83.813, I83.891–I83.893, I83.91–I83.93, I87.001–I87.093 (Excluding codes with "9" as the sixth character), I87.2, I89.0, L97.111–L97.129, L97.211–L97.229, L97.311–L97.329, L97.411–L97.429, L97.511–L97.529, L97.811–L97.829, L97.911–L97.929, O12.00, O12.04, O12.05, O12.20, O12.24, O12.25, O26.00, Q82.0 |
| A6539 |
No |
No |
No |
I83.019, I83.029, I86.1–I86.3, I87.2, I89.0, O12.01–O12.03, O12.04, O12.05, O12.21–O12.23, O12.24, O12.25, O26.01–O26.03, Q82.0 |
| A6540 |
No |
No |
No |
I83.019, I83.029, I86.1–I86.3, I87.2, I89.0, O12.01–O12.03, O12.04, O12.05, O12.21–O12.23, O12.24, O12.25, O26.01–O26.03, Q82.0 |
| A6541 |
No |
No |
No |
I83.019, I83.029, I86.1–I86.3, I87.2, I89.0, O12.01–O12.03, O12.04, O12.05, O12.21–O12.23, O12.24, O12.25, O26.01–O26.03, Q82.0 |
| A6545 |
No |
Yes |
Yes |
I83.019, I83.029, I86.1–I86.3, I87.2, I89.0, O12.01–O12.03, O12.04, O12.05, O12.21–O12.23, O12.24, O12.25, O26.01–O26.03, Q82.0 |
| A6549 |
Yes |
Yes |
Yes |
I83.019, I83.029, I86.1–I86.3, I87.2, I89.0, O12.01–O12.03, O12.04, O12.05, O12.21–O12.23, O12.24, O12.25, O26.01–O26.03, Q82.0 |
| S8420 |
Yes |
Yes |
Yes |
I97.2 |
| S8421 |
No |
Yes |
No |
I97.2 |
| S8422 |
Yes |
Yes |
Yes |
I97.2 |
| S8423 |
Yes |
Yes |
Yes |
I97.2 |
| S8424 |
No |
Yes |
No |
I97.2 |
| S8425 |
Yes |
Yes |
Yes |
I97.2 |
| S8426 |
Yes |
Yes |
Yes |
I97.2 |
| S8427 |
No |
Yes |
No |
I97.2 |
| S8428 |
No |
Yes |
No |
I97.2 |
| S8429 |
Yes |
Yes |
Yes |
I83.011–I83.029, I83.11, I83.12, I83.211–I83.812, I83.891–I83.893, I83.91–I83.93, I86.1–I86.3, I87.001–I87.093 (Excluding codes with "9" as the sixth character), I87.2, I87.9, I89.0, I97.2, O12.01–O12.03, O12.04, O12.05, O12.21–O12.23, O12.24, O12.25, O26.01–O26.03, Q82.0 |
1A "Yes" in this column indicates claim attachments are required with this procedure code. Refer to the Claim Attachment Requirements section below for more information.
2A "Yes" in this column indicates the compression garment must be billed with an RA modifier if the provider is replacing the member's compression garment using measurements currently on file.
3When a member has one of the allowable diagnoses listed for the procedure code, PA is required only if the life expectancy has been exceeded. If the member has an allowable diagnosis for the requested procedure code, the diagnosis code must be entered in the claim's primary diagnosis field. If the member has a diagnosis not included in the listed allowable diagnoses, providers may submit a PA request.
*This code range requires a seventh character. These characters can be "A" for initial encounter, "D" for subsequent encounter, or "S" for sequela. This seventh character must always be preceded by six characters. If more characters are needed for the code to contain seven, an "X" should be used as a placeholder (e.g., T20.00XA).
Claim Attachment Requirements
The use of a "custom" or "not otherwise specified" procedure code for a gradient compression garment on a claim should only be used in exceptional cases. For "custom" or "not otherwise specified" gradient compression garments, each attachment must document why a "custom" or "not otherwise specified" procedure code was used instead of a non-custom compression garment procedure code. All compression burn garments are considered custom and therefore also require attachments to be submitted with the claim.
When using procedure codes marked with a "Yes" under "Claim Attachment" in the table above, ForwardHealth requires the following attachments when submitting claims:
- The physician prescription. Refer to Prescription Requirements for more information.
- The form or document used to record the measurements used for the garment order/fabrication, which includes:
- The date the measurements were taken or date(s) the measurements were re-affirmed, if applicable. If a provider re-affirms the previous measurements, ForwardHealth recommends the provider sign and date the same form used in the previous order if the previous measurements remain accurate.
- The name and credentials of the individual taking or affirming the measurements (i.e., the certified fitter, ABC-certified orthotist or prosthetist, or licensed physical therapist or occupational therapist).
- The provider's justification for the use of a "custom" or "not otherwise specified" procedure code. To justify use of a custom or not otherwise specified procedure code, ForwardHealth recommends identifying the extremity's circumferential measurement that did not allow fitting the member with a garment represented by a specified code by circling the measurement on the form, adding a notation in the margin of the measurement or order form, and/or including a narrative as an additional record. One example of when a custom compression garment may be justified is when the body part or segment is an atypical shape. However, a body part or segment that is simply larger than average would not justify a custom or not otherwise specified compression garment and a specified procedure code should be used on the claim (and attachments should not be submitted).
- The provider invoice with the specific garment(s) clearly identified.
For those claims submitted without PA, the allowable diagnosis code (listed in the table above) and any required modifiers must be on the claim.
Modifiers RT and LT Required on Claims
Providers are required to include modifier RT and/or LT on claims submitted for the procedure codes marked with "Yes" under "RT and/or LT Modifier Required?" in the table (A6504–A6508, A6530–A6538, A6549, and S8420–S8429). Modifier RT is used to reference a garment applied to a right extremity. Modifier LT is used to reference a garment applied to a left extremity. Procedure codes A6504–A6508, A6530–A6538, A6549, and S8420–S8429 are incomplete without modifier RT or LT.
If there is a bilateral need, providers are required to submit two separate details on claims, with modifier RT on one detail line and modifier LT on a second detail line. ForwardHealth will not accept modifier 50 (Bilateral) for processing claims for compression garments.
Claims for pantyhose, waist-high garments, vests, panties, or facial masks should not include the RT and LT modifiers.
Modifier RA for Custom Compression Garment Reorders
If a provider is replacing a member's compression garment using measurements currently on file, the provider is required to use the RA modifier. However, if the garment is being replaced based on new measurements, even if there is no change to the measurements currently on file, the providers should not use the RA modifier.
The use of the RA modifier does not change the requirement to submit supporting documentation with the claim for custom and not otherwise specified procedure codes. Refer to Claim Attachment Requirements for more information.
Providers are reminded that all claims submitted must be supported by records maintained by the provider in accordance with Wis. Admin. Code § DHS 106.02(9)(e)1. In addition, the provider record must include confirmation of delivery of the service or item to the member. For DME, the DOS is the date the item is delivered to the member.
Provider records that do not support the procedure codes listed on the claim are subject to claim denial, reduction in reimbursement, or recoupment.
Claim Submittal Recommendations
If a member requires two different compression garments per body segment, the provider should submit both compression garment procedure codes on one claim with the required supporting documentation.
If a member requires more than one compression garment (e.g., one arm, two legs, and a non-elastic wrap), the provider is urged to submit all the member's required compression garments on one claim, rather than submitting one claim for each garment. While ForwardHealth supports a provider's flexibility in submitting claims, submitting claims as suggested may reduce denials for insufficient documentation (i.e., insufficient to either support the claim or to refute the apparent duplication of services).
Refer to Prior Authorization for Burn and Gradient Compression Garments for information on PA. Topic #4817 Submitting Paper Attachments With Electronic Claims
Providers may submit paper attachments to accompany electronic claims and electronic claim adjustments. Providers should refer to their companion guides for directions on indicating that a paper attachment will be submitted by mail.
Paper attachments that go with electronic claim transactions must be submitted with the Claim Form Attachment Cover Page. Providers are required to indicate an ACN for paper attachment(s) submitted with electronic claims. (The ACN is an alphanumeric entry between 2 and 80 digits assigned by the provider to identify the attachment.) The ACN must be indicated on the cover page so that ForwardHealth can match the paper attachment(s) to the correct electronic claim.
ForwardHealth will hold an electronic claim transaction or a paper attachment(s) for up to seven calendar days to find a match. If a match cannot be made within seven days, the claim will be processed without the attachment and will be denied if an attachment is required. When such a claim is denied, both the paper attachment(s) and the electronic claim will need to be resubmitted.
Providers are required to send paper attachments relating to electronic claim transactions to the following address:
ForwardHealth
Claims and Adjustments
313 Blettner Blvd
Madison WI 53784
This does not apply to compound and noncompound claims. Topic #11677 Uploading Claim Attachments Via the Portal
Providers are able to upload attachments for most claims via the secure Provider area of the ForwardHealth Portal. This allows providers to submit all components for claims electronically.
Providers are able to upload attachments via the Portal when a claim is suspended and an attachment was indicated but not yet received. Providers are able to upload attachments for any suspended claim that was submitted electronically. Providers should note that all attachments for a suspended claim must be submitted within the same business day.
Claim Types
Providers will be able to upload attachments to claims via the Portal for the following claim types:
- Professional.
- Institutional.
- Dental.
The submission policy for compound and noncompound drug claims does not allow attachments.
Document Formats
Providers are able to upload documents in the following formats:
- JPEG (.jpg or .jpeg).
- PDF (.pdf).
- Rich Text Format (.rtf).
- Text File (.txt).
JPEG files must be stored with a ".jpg" or ".jpeg" extension; text files must be stored with a ".txt" extension; rich text format files must be stored with a ".rtf" extension; and PDF files must be stored with a ".pdf" extension.
Microsoft Word files (.doc) cannot be uploaded but can be saved and uploaded in Rich Text Format or Text File formats.
Uploading Claim Attachments
Claims Submitted by Direct Data Entry
When a provider submits a DDE claim and indicates an attachment will also be included, a feature button will appear and link to the DDE claim screen where attachments can be uploaded.
Providers are still required to indicate on the DDE claim that the claim will include an attachment via the "Attachments" panel.
Claims will suspend for seven days before denying for not receiving the attachment.
Claims Submitted by Provider Electronic Software and 837 Health Care Claim Transactions
Providers submitting claims via 837 transactions are required to indicate attachments via the PWK segment. Providers submitting claims via PES software will be required to indicate attachments via the attachment control field. Once the claim has been submitted, providers will be able to search for the claim on the Portal and upload the attachment via the Portal. Refer to the Implementation Guides for how to use the PWK segment in 837 transactions and the PES Manual for how to use the attachment control field.
Claims will suspend for seven days before denying for not receiving the attachment. |