| Program Name: | BadgerCare Plus and Medicaid | Handbook Area: | HealthCheck (EPSDT) | | 04/23/2024 | Claims : SubmissionTopic #4577 American Dental Association 2006 Claim Form Completion Instructions
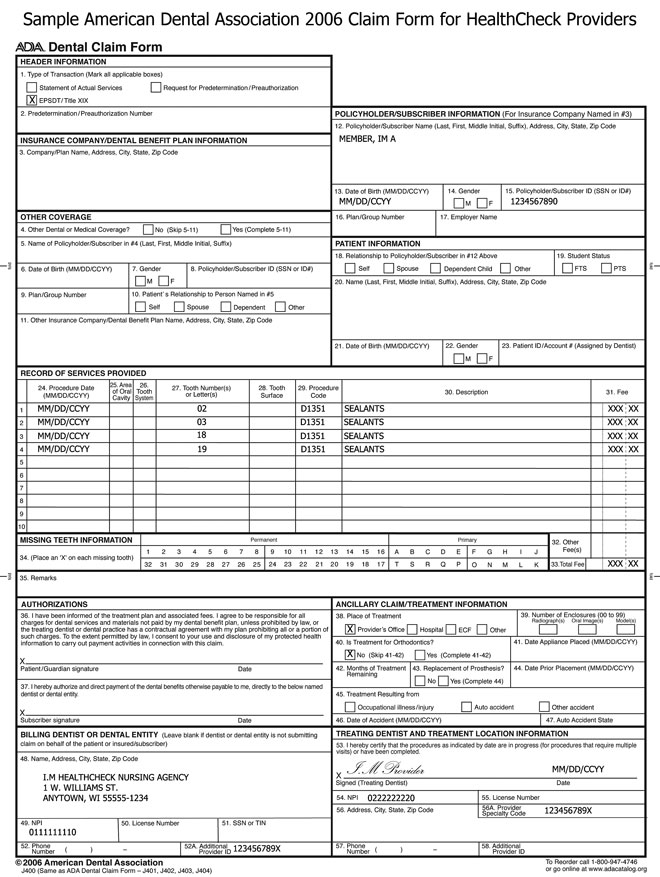
A sample ADA 2006 claim form is available for HealthCheck providers.
Use the following claim form completion instructions, not the claim form's printed descriptions, to avoid denial or inaccurate claim payment. Complete all required elements as appropriate. Be advised that every code used, even if it is entered in a non-required element, is required to be a valid code. Do not include attachments unless instructed to do so.
Members enrolled in BadgerCare Plus or Medicaid receive a ForwardHealth ID card. Always verify a member's enrollment before providing
nonemergency services to determine if there are any limitations on covered services and to obtain the correct spelling of the member's name.
When submitting a claim with multiple pages, providers are required to indicate page numbers using the format "Page X of X" in the upper right corner of the claim form.
Submit completed single-page paper claims to the following address:
ForwardHealth
Claims and Adjustments
313 Blettner Blvd
Madison WI 53784
Submit completed multiple-page paper claims to the following address:
ForwardHealth
Multiple-Page Dental Claims
Ste 22
313 Blettner Blvd
Madison WI 53784
HEADER INFORMATION
Element1 —Type of Transaction (required, if applicable)
EPSDT (HealthCheck): HealthCheck is Wisconsin Medicaid's federally mandated program known nationally as EPSDT. If the services were performed as a result of a HealthCheck/EPSDT exam, check the EPSDT box.
Element 2—Predetermination/Preauthorization Number (not required)
INSURANCE COMPANY/DENTAL BENEFIT PLAN INFORMATION
Element 3—Company/Plan Name, Address, City, State, Zip Code (not required)
OTHER COVERAGE
Element 4—Other Dental or Medical Coverage? (not required)
Element 5—Name of Policyholder/Subscriber in #4 (Last, First, Middle Initial, Suffix) (not required)
Element 6—Date of Birth (MM/DD/CCYY) (not required)
Element 7—Gender (not required)
Element 8—Policyholder/Subscriber ID (SSN or ID#) (not required)
Element 9—Plan/Group Number (not required)
Element 10—Patient's Relationship to Person Named in #5 (not required)
Element 11—Other Insurance Company/Dental Benefit Plan Name, Address, City, State, Zip Code
Except for a few instances, ForwardHealth is the payer of last resort for any services covered by ForwardHealth. This means the provider is required to make a reasonable effort to exhaust all existing other health insurance sources before billing ForwardHealth unless the service is not covered by other health insurance. Element 11 identifies Medicare and commercial health insurance and whether the member has commercial health insurance coverage, Medicare coverage, or both.
There are specific instructions for each coverage type. Providers should use the following guidelines for this element depending on the member's coverage:
- Members with commercial health insurance coverage
- Members with Medicare coverage
- Members with both Medicare and commercial health insurance coverage
Members with Commercial Health Insurance Coverage
Commercial health insurance coverage must be billed prior to submitting claims to ForwardHealth, unless the service does not require commercial health insurance billing as determined by ForwardHealth. Commercial health insurance coverage is indicated by Wisconsin's EVS under "Other Commercial Health Insurance." ForwardHealth has defined a set of "other insurance" indicators. Additionally, ForwardHealth has identified specific CDT codes that must be billed to other health insurance sources prior to being billed to ForwardHealth.
Note: When commercial health insurance paid only for some services (or applied a payment to the member's cost share) and denied payment for the others, ForwardHealth recommends that providers submit two separate claims. To maximize reimbursement, one
claim should be submitted for the partially paid services and another claim should be submitted for the services that were denied.
The following table indicates appropriate other insurance codes for use in Element 11.
| Code |
Description |
| OI-P |
PAID in part or in full by commercial health insurance and/or was applied toward the deductible, coinsurance, copayment, blood deductible, or psychiatric reduction. Indicate the amount paid by commercial health insurance to the provider or
to the insured. |
| OI-D |
DENIED by commercial health insurance following submission of a correct and complete claim. Do not use this code unless the claim was actually billed to the commercial health insurer. |
| OI-Y |
YES, the member has commercial health insurance coverage, but it was not billed for reasons including, but not limited to, the following:
- The member denied coverage or will not cooperate.
- The provider knows the service in question is not covered by the carrier.
- The member's commercial health insurance failed to respond to initial and follow-up claims.
- Benefits are not assignable or cannot get assignment.
- Benefits are exhausted.
|
Note: The provider may not use OI-D or OI-Y if the member is covered by a commercial HMO and the HMO denied payment because an otherwise covered service was not rendered by a designated provider. Services covered by a commercial HMO are not reimbursable by ForwardHealth except for the copayment and deductible amounts. Providers who receive a capitation payment from the commercial HMO may not bill ForwardHealth for services that are included in the capitation payment.
Members with Medicare Coverage
Submit claims to Medicare before submitting claims to ForwardHealth.
Do not enter a Medicare disclaimer code in Element 11 when one or more of the following statements is true:
- Medicare never covers the procedure in any circumstance.
- ForwardHealth indicates the member does not have any Medicare coverage,
including a Medicare Advantage Plan, for the service
provided. For example, the service is covered by Medicare Part A, but the
member does not have Medicare Part A.
- ForwardHealth indicates that the provider is not Medicare enrolled.
- Medicare has allowed the charges. In this case, attach the EOMB, but do not indicate on the claim form the amount Medicare paid.
If none of the previous statements is true, a Medicare disclaimer code is necessary. The following table indicates appropriate Medicare disclaimer codes for use in Element 11 when billing Medicare prior to billing ForwardHealth.
| Code |
Description |
| M-7 |
Medicare disallowed or denied payment. This code applies when Medicare denies the claim for reasons related to policy
(not billing errors), or the member's lifetime benefit, SOI, or yearly allotment of available benefits is exhausted.
For Medicare Part A, use M-7 in the following instances (all three criteria must be met):
- The provider is identified in ForwardHealth files as enrolled in Medicare Part A.
- The member is eligible for Medicare Part A.
- The service is covered by Medicare Part A but is denied by Medicare Part A due to frequency limitations, diagnosis restrictions, or exhausted
benefits.
For Medicare Part B, use M-7 in the following instances (all three criteria must be met):
- The provider is identified in ForwardHealth files as enrolled in Medicare Part B.
- The member is eligible for Medicare Part B.
- The service is covered by Medicare Part B but is denied by Medicare Part B due to frequency limitations, diagnosis restrictions, or exhausted
benefits.
|
| M-8 |
Noncovered Medicare service. This code may be used when Medicare was not billed because the service is not covered in this circumstance.
For Medicare Part A, use M-8 in the following instances (all three criteria must be met):
- The provider is identified in ForwardHealth files as enrolled in Medicare Part A.
- The member is eligible for Medicare Part A.
- The service is usually covered by Medicare Part A but not in this circumstance (for example, member's diagnosis).
For Medicare Part B, use M-8 in the following instances (all three criteria must be met):
- The provider is identified in ForwardHealth files as enrolled in Medicare Part B.
- The member is eligible for Medicare Part B.
- The service is usually covered by Medicare Part B but not in this circumstance (for example, member's diagnosis).
|
Members with Both Medicare and Commercial Health Insurance Coverage
Use both a Medicare disclaimer code ("M-7" or "M-8") and an other insurance indicator code (for example, "OI-P") when applicable.
POLICYHOLDER/SUBSCRIBER INFORMATION
Element 12—Policyholder/Subscriber Name (First, Last, Middle Initial, Suffix), Address, City, State, Zip Code
Enter the member's last name, first name, and middle initial. Use the EVS to obtain the correct spelling of the member's name. If the name or spelling of the name on the ForwardHealth card and the EVS do not match, use the spelling from the EVS. The member's address, city, state, and zip code are not required.
Element 13—Date of Birth
Enter the member's birth date in MM/DD/CCYY format.
Element 14—Gender (not required)
Element 15—Policyholder/Subscriber ID (SSN or ID#)
Enter the member ID number. Do not enter any other numbers or letters. Use the ForwardHealth card or the EVS to obtain the correct member ID.
Element 16—Plan/Group Number (not required)
Element 17—Employer Name (not required)
PATIENT INFORMATION
Element 18—Relationship to Policyholder/Subscriber in #12 Above (not required)
Element 19—Student Status (not required)
Element 20—Name (Last, First, Middle Initial, Suffix), Address, City, State, Zip Code (not required)
Element 21—Date of Birth (MM/DD/CCYY) (not required)
Element 22—Gender (not required)
Element 23—Patient ID/Account # (Assigned by Dentist) (not required)
RECORD OF SERVICES PROVIDED
Element 24—Procedure Date (MM/DD/CCYY)
Enter the DOS in MM/DD/CCYY format for each detail.
Element 25—Area of Oral Cavity
If the procedure applies to gingivectomy, perio scaling, repair of dentures or partials, alveoplasty, or fixed bilateral space maintenance, the area of the oral cavity is entered here.
Element 26—Tooth System (not required)
Element 27—Tooth Number(s) or Letter(s)
If the procedure applies to only one tooth, the tooth number or tooth letter is entered here.
Element 28—Tooth Surface
Enter the tooth surface(s) restored for each restoration.
Element 29—Procedure Code
Enter the appropriate procedure code for each dental service provided.
Element 30—Description
Write a brief description of each procedure.
Element 31—Fee
Enter the usual and customary charge for each detail line of service.
Element 32—Other Fee(s) (required for other insurance information, if applicable)
Enter the actual amount paid by commercial health insurance. (If the dollar amount indicated in Element 32 is greater than zero, and/or was applied toward the deductible, coinsurance, copayment, blood deductible, or psychiatric reduction, "OI-P" must be
indicated in Element 11.) Do not include the deductible, coinsurance, copayment, blood deductible, or psychiatric reduction amount within Element 32. If the commercial health insurance plan paid on only some services, those partially paid services should be submitted on a separate claim from the unpaid services to maximize reimbursement. This allows ForwardHealth to appropriately credit the payments. If the commercial health insurance denied the claim, enter "000." Do not enter Medicare-paid amounts in this field.
Element 33—Total Fee
Enter the total of all detail charges. Do not subtract other insurance payments.
MISSING TEETH INFORMATION
Element 34—Permanent and Primary (Place an "X" on each missing tooth) (not required)
Element 35—Remarks (required, if applicable)
List any unusual services, including reasons why limitations were exceeded.
Providers should enter the word "Emergency" in this element for an emergency service.
AUTHORIZATIONS
Element 36—Patient/Guardian Signature and Date (not required)
Element 37—Subscriber Signature and Date (not required)
ANCILLARY CLAIM/TREATMENT INFORMATION
Element 38—Place of Treatment (Check applicable box)
Check the appropriate box.
Element 39—Number of Enclosures (00 to 99) (not required)
Element 40—Is Treatment for Orthodontics? (not required)
Element 41—Date Appliance Placed (MM/DD/CCYY) (not required)
Element 42—Months of Treatment Remaining (not required)
Element 43—Replacement of Prosthesis? (not required)
Element 44—Date Prior Placement (MM/DD/CCYY) (not required)
Element 45—Treatment Resulting from (Check applicable box) (required, if applicable)
Check the appropriate box if the dental services were the result of an occupational illness/injury, auto accident, or other accident.
Element 46—Date of Accident (MM/DD/CCYY) (required, if applicable)
If a box was checked in Element 45, enter the date the accident happened.
Element 47—Auto Accident State (required, if applicable)
Enter the state where the auto accident occurred.
BILLING DENTIST OR DENTAL ENTITY
Element 48—Name, Address, City, State, Zip Code
Enter the name of the provider submitting the claim and the complete mailing address. The minimum requirement is the provider's name, street, city, state, and zip+4 code. If the billing provider is a group or clinic, enter the group or clinic name in this element. The name in Element 48 must correspond with the NPI in Element 49.
Element 49—NPI
Enter the NPI of the billing provider. The NPI in this element must correspond with the provider name indicated in Element 48.
Element 50—License Number (not required)
Element 51—SSN or TIN (not required)
Element 52—Phone Number (not required)
Element 52A—Additional Provider ID
Enter the billing provider's 10-digit taxonomy code. The taxonomy code in this element must correspond with the NPI indicated in Element 49.
TREATING DENTIST AND TREATMENT LOCATION INFORMATION
Element 53—Dentist's Signature and Date
The provider or the authorized representative must sign in Element 53. The month, day, and year the form is signed must also be entered in MM/DD/CCYY format.
Note: The signature may be a computer-printed or typed name and date or a signature stamp with a date. However, claims with "signature on file" stamps are denied.
Element 54—NPI (required, if applicable)
If the treating provider's NPI is different than the billing provider NPI in Element 49, enter the treating provider's NPI in this element.
Element 55—License Number (not required)
Element 56—Address, City, State, Zip Code (not required)
Element 56A—Provider Specialty Code (required, if applicable)
Enter the treating provider's 10-digit taxonomy code. The taxonomy code in this element must correspond with the NPI indicated in Element 54.
Element 57—Phone Number (not required)
Element 58—Additional Provider ID (not required)
 |