| Program Name: | BadgerCare Plus and Medicaid | Handbook Area: | Durable Medical Equipment | | 04/17/2024 | Member Information : Enrollment CategoriesTopic #225 BadgerCare Plus
Populations Eligible for BadgerCare Plus
The following populations are eligible for BadgerCare Plus:
- Parents and caretakers with incomes at or below 100 percent of the FPL
- Pregnant women with incomes at or below 300 percent of the FPL
- Children (ages 18 and younger) with household incomes at or below 300 percent of the FPL
- Childless adults with incomes at or below 100 percent of the FPL
- Transitional medical assistance individuals, also known as members on extensions, with incomes over 100 percent of the FPL
Where available, BadgerCare Plus members are enrolled in BadgerCare Plus HMOs. In those areas of Wisconsin where HMOs are not available, services will be reimbursed on a fee-for-service basis.
Premiums
The following members are required to pay premiums to be enrolled in BadgerCare Plus:
- Transitional medical assistance individuals with incomes over 133 percent of the FPL. Transitional medical assistance individuals with incomes between 100 and 133 percent FPL are exempt from premiums for the first six months of their eligibility period.
- Children (ages 18 and younger) with household incomes greater than 200 percent with the following exceptions:
- Children under age 1 year.
- Children who are tribal members or otherwise eligible to receive Indian Health Services.
Topic #16677 BadgerCare Plus Benefit Plan Changes
Effective April 1, 2014, all members eligible for BadgerCare Plus were enrolled in the BadgerCare Plus Standard Plan. As a result of this change, the following benefit plans were discontinued:
- BadgerCare Plus Benchmark Plan
- BadgerCare Plus Core Plan
- BadgerCare Plus Basic Plan
Members who are enrolled in the Benchmark Plan or the Core Plan who met new income limits for BadgerCare Plus eligibility were automatically transitioned into the BadgerCare Plus Standard Plan on April 1, 2014. In addition, the last day of BadgerRx Gold program coverage for all existing members was March 31, 2014.
Providers should refer to the March 2014 Online Handbook archive of the appropriate service area for policy information pertaining to these discontinued benefit plans. Topic #785 BadgerCare Plus Prenatal Program
As a result of 2005 Wisconsin Act 25, BadgerCare has expanded coverage to the following individuals:
- Pregnant non-U.S. citizens who are not qualified aliens but meet other eligibility criteria for BadgerCare.
- Pregnant individuals detained by legal process who meet other eligibility criteria for BadgerCare.
The BadgerCare Plus Prenatal Program is designed to provide better birth outcomes.
Women are eligible for all covered services from the first of the month in which their pregnancy is verified or the first of the month in which the application for BadgerCare Plus is filed, whichever is later. Members are enrolled through the last day of the month in which they deliver or the pregnancy ends. Postpartum care is reimbursable only if provided as part of global obstetric care. Even though enrollment is based on pregnancy, these women are eligible for all covered services. (They are not limited to pregnancy-related services.)
These women are not presumptively eligible. Providers should refer them to the appropriate income maintenance or tribal agency where they can apply for this coverage.
Fee-for-Service
Pregnant non-U.S. citizens who are not qualified aliens and pregnant individuals detained by legal process receive care only on a fee-for-service basis. Providers are required to follow all program requirements (e.g., claim submission procedures, PA requirements) when providing services to these women.
Emergency Services for Non-U.S. Citizens
When BadgerCare Plus enrollment ends for pregnant non-U.S. citizens who are not qualified aliens, they receive coverage for emergency services. These women receive emergency coverage for 60 days after the pregnancy ends; this coverage continues through the end of the month in which the 60th day falls (e.g., a woman who delivers on June 20, 2006, would be enrolled through the end of August 2006). Topic #230 Express Enrollment for Children and Pregnant Women
The EE for Pregnant Women Benefit is a limited benefit category that allows a pregnant woman to receive immediate pregnancy-related outpatient services while her application for full-benefit BadgerCare Plus is processed. Enrollment is not restricted based on the member's other health insurance coverage. Therefore, a pregnant woman who has other health insurance may be enrolled in the benefit.
The EE for Children Benefit allows certain members through 18 years of age to receive BadgerCare Plus benefits while an application for BadgerCare Plus is processed.
Fee-for-Service
Women and children who are temporarily enrolled in BadgerCare Plus through the EE process are not eligible for enrollment in an HMO until they are determined eligible for full benefit BadgerCare Plus by the income maintenance or tribal agency. Topic #226 Family Planning Only Services
Family Planning Only Services is a limited benefit program that provides routine contraceptive management or related services to low-income individuals who are of childbearing/reproductive age (typically 15 years of age or older) and who are otherwise not eligible for Wisconsin Medicaid or BadgerCare Plus. Members receiving Family Planning Only Services must be receiving routine contraceptive management or related services.
Note: Members who meet the enrollment criteria may receive routine contraceptive management or related services immediately by temporarily enrolling in Family Planning Only Services through EE.
The goal of Family Planning Only Services is to provide members with information and services to assist them in preventing pregnancy, making BadgerCare Plus enrollment due to pregnancy less likely. Providers should explain the purpose of Family Planning Only Services to members and encourage them to contact their certifying agency to determine their enrollment options if they are not interested in, or do not need, contraceptive services.
Members enrolled in Family Planning Only Services receive routine services to prevent or delay pregnancy and are not eligible for other services (e.g., PT services, dental services). Even if a medical condition is discovered during a family planning visit, treatment for the condition is not covered under Family Planning Only Services unless the treatment is identified in the list of allowable procedure codes for Family Planning Only Services.
Members are also not eligible for certain other services that are covered under Wisconsin Medicaid and BadgerCare Plus (e.g., mammograms and hysterectomies). If a medical condition, other than an STD, is discovered during routine contraceptive management or related services, treatment for the medical condition is not covered under Family Planning Only Services.
Colposcopies and treatment for STDs are only covered through Family Planning Only Services if they are determined medically necessary during routine contraceptive management or related services. A colposcopy is a covered service when an abnormal result is received from a pap test, prior to the colposcopy, while the member is enrolled in Family Planning Only Services and receiving contraceptive management or related services.
Family Planning Only Services members diagnosed with cervical cancer, precancerous conditions of the cervix, or breast cancer may be eligible for Wisconsin Well Woman Medicaid. Providers should assist eligible members with the enrollment process for Well Woman Medicaid.
Providers should inform members about other coverage options and provide referrals for care not covered by Family Planning Only Services. Topic #4757 ForwardHealth and ForwardHealth interChange
ForwardHealth brings together many Wisconsin DHS health care programs with the goal to create efficiencies for providers and to improve health outcomes for members. ForwardHealth interChange is the DHS claims processing system that supports multiple state health care programs and web services, including:
- BadgerCare Plus
- BadgerCare Plus and Medicaid managed care programs
- SeniorCare
- ADAP
- WCDP
- WIR
- Wisconsin Medicaid
- Wisconsin Well Woman Medicaid
- WWWP
ForwardHealth interChange is supported by the state's fiscal agent, Gainwell Technologies. Topic #229 Limited Benefit Categories Overview
Certain members may be enrolled in a limited benefit category. These limited benefit categories include the following:
- BadgerCare Plus Prenatal Program
- EE for Children
- EE for Pregnant Women
- Family Planning Only Services, including EE for individuals applying for Family Planning Only Services
- QDWI
- QI-1
- QMB Only
- SLMB
- Tuberculosis-Related Medicaid
Members may be enrolled in full-benefit Medicaid or BadgerCare Plus and also be enrolled in certain limited benefit programs, including QDWI, QI-1, QMB Only, and SLMB. In those cases, a member has full Medicaid or BadgerCare Plus coverage in addition to limited coverage for Medicare expenses.
Members enrolled in the BadgerCare Plus Prenatal Program, Family Planning Only Services, EE for Children, EE for Pregnant Women, or Tuberculosis-Related Medicaid cannot be enrolled in full-benefit Medicaid or BadgerCare Plus. These members receive benefits through the limited benefit category.
Providers should note that a member may be enrolled in more than one limited benefit category. For example, a member may be enrolled in Family Planning Only Services and Tuberculosis-Related Medicaid.
Providers are strongly encouraged to verify dates of enrollment and other coverage information using Wisconsin's EVS to determine whether a member is in a limited benefit category, receives full-benefit Medicaid or BadgerCare Plus, or both.
Providers are responsible for knowing which services are covered under a limited benefit category. If a member of a limited benefit category requests a service that is not covered under the limited benefit category, the provider may collect payment from the member if certain conditions are met. Topic #228 Medicaid
Medicaid is a joint federal/state program established in 1965 under Title XIX of the Social Security Act to pay for medical services for selected groups of people who meet the program's financial requirements.
The purpose of Medicaid is to provide reimbursement for and assure the availability of appropriate medical care to persons who meet the criteria for Medicaid. Wisconsin Medicaid is also known as the Medical Assistance Program, WMAP, MA, Title XIX, or T19.
A Medicaid member is any individual entitled to benefits under Title XIX of the Social Security Act and under the Medical Assistance State Plan as defined in Wis. Stat. ch. 49.
Wisconsin Medicaid enrollment is determined on the basis of financial need and other factors. A citizen of the United States or a "qualified immigrant" who meets low-income financial requirements may be enrolled in Wisconsin Medicaid if they are in one of the following categories:
- Age 65 and older
- Blind
- Disabled
Some needy and low-income people become eligible for Wisconsin Medicaid by qualifying for programs such as:
- Katie Beckett
- Medicaid Purchase Plan
- Foster care or adoption assistance programs
- SSI
- WWWP
Providers may advise these individuals or their representatives to contact their certifying agency for more information. The following agencies certify people for Wisconsin Medicaid enrollment:
- Income maintenance or tribal agencies
- Medicaid outstation sites
- SSA offices
In limited circumstances, some state agencies also certify individuals for Wisconsin Medicaid.
Medicaid fee-for-service members receive services through the traditional health care payment system under which providers receive a payment for each unit of service provided. Some Medicaid members receive services through state-contracted MCOs. Topic #232 Qualified Disabled Working Individual Members
QDWI members are a limited benefit category of Medicaid members. They receive payment of Medicare monthly premiums for Part A.
QDWI members are certified by their income maintenance or tribal agency. To qualify, QDWI members are required to meet the following qualifications:
- Have income under 200 percent of the FPL
- Be entitled to, but not necessarily enrolled in, Medicare Part A
- Have income or assets too high to qualify for QMB-Only and SLMB
Topic #234 Qualified Medicare Beneficiary-Only Members
QMB-Only members are a limited benefit category of Medicaid members. They receive payment of the following:
- Medicare monthly premiums for Part A, Part B, or both
- Coinsurance, copayment, and deductible for Medicare-allowed services
QMB-Only members are certified by their income maintenance or tribal agency. QMB-Only members are required to meet the following qualifications:
- Have an income under 100 percent of the FPL
- Be entitled to, but not necessarily enrolled in, Medicare Part A
Topic #235 Qualifying Individual 1 Members
QI-1 members are a limited benefit category of Medicaid members. They receive payment of Medicare monthly premiums for Part B.
QI-1 members are certified by their income maintenance or tribal agency. To qualify, QI-1 members are required to meet the following qualifications:
- Have income between 120 and 135 percent of the FPL
- Be entitled to, but not necessarily enrolled in, Medicare Part A
Topic #18777 Real-Time Eligibility Determinations
ForwardHealth may complete real-time eligibility determinations for BadgerCare Plus and/or Family Planning Only Services applicants who meet pre-screening criteria and whose reported information can be verified in real time while applying in ACCESS Apply for Benefits. Once an applicant is determined eligible through the real-time eligibility process, they are considered eligible for BadgerCare Plus and/or Family Planning Only Services and will be enrolled for 12 months, unless changes affecting eligibility occur before the 12-month period ends.
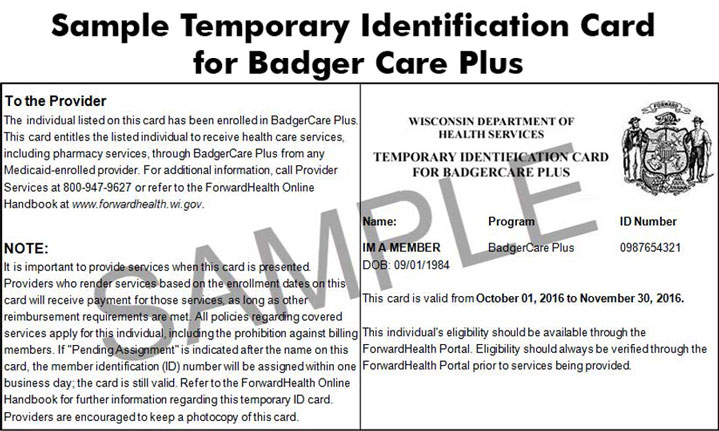
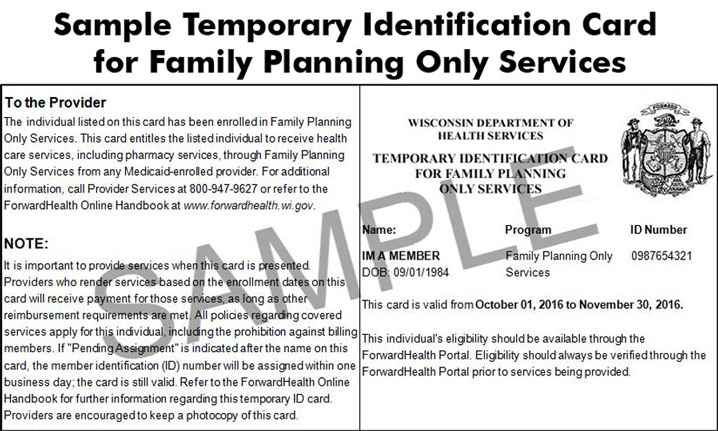
A member determined eligible through the real-time eligibility process will receive a temporary ID card for BadgerCare Plus and/or Family Planning Only Services. Each member will get their own card, and each card will include the member's ForwardHealth ID number. The temporary ID card will be valid for the dates listed on the card and will allow the member to get immediate health care or pharmacy services.
Eligibility Verification
When a member is determined eligible for BadgerCare Plus and/or Family Planning Only Services through the real-time eligibility process, providers are able to see the member's eligibility information in Wisconsin's EVS in real time. Providers should always verify eligibility through EVS prior to providing services.
On rare occasions, it may take up to 48 hours for eligibility information to be available through interChange. In such instances, if a member presents a valid temporary ID card, the provider is still required to provide services, even if eligibility cannot be verified through EVS.
 Topic #236 Specified Low-Income Medicare Beneficiaries
SLMB members are a limited benefit category of Medicaid members. They receive payment of Medicare monthly premiums for Part B.
SLMB members are certified by their income maintenance or tribal agency. To qualify, SLMB members are required to meet the following qualifications:
- Have an income under 120 percent of the FPL
- Be entitled to, but not necessarily enrolled in, Medicare Part A
Topic #262 Tuberculosis-Related Medicaid
Tuberculosis-Related Medicaid is a limited benefit category that allows individuals with TB infection or disease to receive covered TB-related outpatient services. Topic #240 Wisconsin Well Woman Medicaid
Wisconsin Well Woman Medicaid provides full Medicaid benefits to underinsured or uninsured women ages 35 to 64 who have been screened and diagnosed by WWWP or Family Planning Only Services, meet all other enrollment requirements, and are in need of treatment for any of the following:
- Breast cancer
- Cervical cancer
- Precancerous conditions of the cervix
Services provided to women who are enrolled in WWWMA are reimbursed through Medicaid fee-for-service. |