| Program Name: | BadgerCare Plus and Medicaid | Handbook Area: | Disposable Medical Supplies | | 04/23/2024 | Prior Authorization : Forms and AttachmentsTopic #960 An Overview
Depending on the service being requested, most PA requests must be comprised of the following:
Topic #13137 Enteral Nutrition Formula
The following must be submitted for PA requests for enteral nutrition formula:
- A PA/RF
- A PA/ENFA
- A copy of the original prescription or order that is not greater than one year old
- Supporting clinical documentation that cannot be sufficiently indicated on the PA/ENFA
Billing providers or authorized representatives acting on behalf of billing providers are responsible for the following:
- Obtaining clinical documentation and information from prescribers necessary to submit PA requests (Billing providers may have prescribers complete sections of the PA/ENFA if needed.)
- Signing the PA/RF and PA/ENFA
- The truthfulness, accuracy, timeliness, and completeness of PA requests and submission of PA requests to ForwardHealth
Enteral Nutrition Supplies
ForwardHealth covers enteral feeding supplies up to a maximum quantity per month without PA. Providers may refer to the DMS Index for quantity limits.Topic #446 Attachments
In addition to the PA/RF, PA/HIAS1, or PA/DRF, a service-specific PA attachment must be submitted with each PA request. The PA attachment allows a provider to document the clinical information used to determine whether or not the standards of medical necessity are met for the requested service(s). Providers should include adequate information for ForwardHealth to make a reasonable judgment about the case.
ForwardHealth will scan each form with a barcode as it is received, which will allow greater efficiencies for processing PA requests. Topic #9137 Prior Authorization Drug Attachment for Blood Glucose Meters and Test Strips
Providers requesting PA for Blood Glucose Meters and Test Strips should submit the Prior Authorization Drug Attachment for Blood Glucose Meters and Test Strips along with the PA/RF to ForwardHealth. Topic #1613 Prior Authorization Durable Medical Equipment Attachment
Providers requesting PA for DMS should submit the PA/DMEA along with the PA/RF to ForwardHealth. Topic #447 Obtaining Forms and Attachments
Providers may obtain paper versions of all PA forms and attachments. In addition, providers may download and complete most PA attachments from the ForwardHealth Portal.
Paper Forms
Paper versions of all PA forms and PA attachments are available by writing to ForwardHealth. Include a return address, the name of the form, the form number (if applicable), and mail the request to the following address:
ForwardHealth
Form Reorder
313 Blettner Blvd
Madison WI 53784
Providers may also call Provider Services to order paper copies of forms.
Downloadable Forms
Most PA attachments can be downloaded and printed in their original format from the Portal. Many forms are available in fillable PDF and fillable Microsoft Word formats.
Web PA Via the Portal
Certain providers may complete the PA/RF and PA attachments through the Portal. Providers may then print the PA/RF (and in some cases the PA attachment), and send the PA/RF, service-specific PA attachments, and any supporting documentation on paper by mail or fax to ForwardHealth. Topic #448 Prior Authorization Request Form
The PA/RF is used by ForwardHealth and is mandatory for most providers when requesting PA. The PA/RF serves as the cover page of a PA request.
Providers are required to complete the basic provider, member, and service information on the PA/RF. Each PA request is assigned a unique ten-digit number. ForwardHealth remittance information will report to the provider the PA number used to process the claim for prior authorized services. Topic #1612 Prior Authorization Request Form Completion Instructions for Disposable Medical Supplies
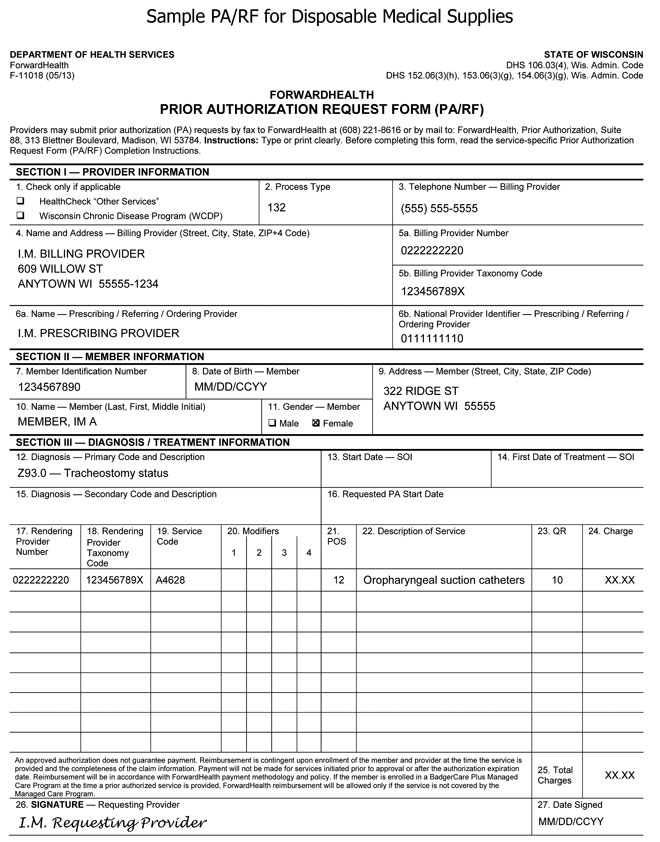
A sample PA/RF for DMS is available.
ForwardHealth requires certain information to enable the programs to authorize and pay for medical services provided to eligible members.
Members of ForwardHealth are required to give providers full, correct, and truthful information for the submission of correct and complete claims for
reimbursement. This information should include, but is not limited to, information concerning enrollment status, accurate name, address, and member
identification number (Wis. Admin. Code § DHS 104.02[4]).
Under Wis. Stat. § 49.45(4), personally identifiable information about program applicants and members is confidential and is used for purposes directly related to ForwardHealth administration such as determining eligibility of the applicant, processing PA requests, or processing provider claims for reimbursement. The use of the PA/RF is mandatory to receive PA for certain items. Failure to supply the information requested by the form may result in denial of PA or payment for the service.
Providers should make duplicate copies of all paper documents mailed to ForwardHealth. Providers may submit PA requests, along with the PA/DMEA by fax to ForwardHealth at 608-221-8616 or by mail to the following address:
ForwardHealth
Prior Authorization
Ste 88
313 Blettner Blvd
Madison WI 53784
The provision of services that are greater than or significantly different from those authorized may result in nonpayment of the billing claim(s).
SECTION I ― PROVIDER INFORMATION
Element 1 — HealthCheck "Other Services" and Wisconsin Chronic Disease Program (WCDP)
Enter an "X" in the box next to HealthCheck "Other Services" if the services requested on the PA/RF are for HealthCheck "Other Services." Enter an "X" in the box next to WCDP if the services requested on the PA/RF are for a WCDP member.
Element 2 — Process Type
Enter the appropriate three-digit process type from the list below. The process type is a three-digit code used to identify a category of service requested. PA requests will be returned without adjudication if no process type is indicated.
132 — DMS
139 — Respiratory equipment
Element 3 — Telephone Number — Billing Provider
Enter the telephone number, including the area code, of the office, clinic, facility, or place of business of the billing provider.
Element 4 — Name and Address — Billing Provider
Enter the name and complete address (street, city, state, and ZIP+4 code) of the billing provider. Providers are required to include both the ZIP code and the four-digit extension for timely and accurate billing. The name listed in this element must correspond with the billing provider number listed in Element 5a.
Element 5a — Billing Provider Number
Enter the provider ID of the billing provider. The provider ID in this element must correspond with the provider name listed in Element 4.
Element 5b — Billing Provider Taxonomy Code
Enter the national 10-digit alphanumeric taxonomy code that corresponds to the billing provider ID in Element 5a.
Note: Providers who are not required to use a NPI should not fill out this field.
Element 6a — Name — Prescribing / Referring / Ordering Provider
Enter the prescribing provider's name.
Element 6b — National Provider Identifier — Prescribing / Referring / Ordering Provider
Enter the prescribing provider's 10-digit NPI.
SECTION II ― MEMBER INFORMATION
Element 7 — Member Identification Number
Enter the member ID. Do not enter any other numbers or letters. Use the ForwardHealth identification card or Wisconsin's EVS to obtain the correct number.
Element 8 — Date of Birth — Member
Enter the member's date of birth in MM/DD/CCYY format.
Element 9 — Address — Member
Enter the complete address of the member's place of residence, including the street, city, state, and ZIP code. If the member is a resident of a nursing home or other facility, include the name of the nursing home or facility.
Element 10 — Name — Member
Enter the member's last name, followed by his or her first name and middle initial. Use the EVS to obtain the correct spelling of the member's name. If the name or spelling of the name on the ForwardHealth card and the EVS do not match, use the spelling from the EVS.
Element 11 — Gender — Member
Enter an "X" in the appropriate box to specify male or female.
SECTION III ― DIAGNOSIS / TREATMENT INFORMATION
Element 12 — Diagnosis — Primary Code and Description
Enter the appropriate ICD diagnosis code and description with the highest level of specificity most relevant to the service/procedure requested. The ICD diagnosis code must correspond with the ICD description.
Element 13 — Start Date — SOI (not required)
Element 14 — First Date of Treatment — SOI (not required)
Element 15 — Diagnosis — Secondary Code and Description
Enter the appropriate secondary ICD diagnosis code and description with the highest level of specificity most relevant to the service/procedure requested, if applicable. The ICD diagnosis code must correspond with the ICD description.
Element 16 — Requested PA Start Date (not required)
Element 17 — Rendering Provider Number
Enter the provider ID of the provider who will be performing the service, only if this number is different from the billing provider ID listed in Element 5a.
Element 18 — Rendering Provider Taxonomy Code
Enter the national 10-digit alphanumeric taxonomy code that corresponds to the provider who will be performing the service, only if this code is different from the taxonomy code listed for the billing provider in Element 5b.
Note: Providers who are not required to use an NPI should not fill out this field.
Element 19 — Service Code
Enter the appropriate HCPCS code for each service/item requested.
Element 20 — Modifiers
Enter the modifier(s) corresponding to the service code listed if a modifier is required.
Element 21 — POS
Enter the appropriate POS code designating where the requested service/item would be provided/performed/dispensed.
Element 22 — Description of Service
Enter a written description corresponding to the appropriate HCPCS code for each service/item requested.
Element 23 — QR
Enter the appropriate quantity (for example, number of services, days' supply) requested for the procedure code listed.
Element 24 — Charge
Enter the provider's usual and customary charge for each service/procedure/item requested. If the quantity is greater than "1.0," multiply the quantity by the charge for each service/procedure/item requested. Enter that total amount in this element.
Note: The charges indicated on the request form should reflect the provider's usual and customary charge for the procedure requested. Providers are reimbursed for authorized services according to provider Terms of Reimbursement issued by the DHS.
Element 25 — Total Charges
Enter the anticipated total charges for this request.
Element 26 — Signature — Requesting Provider
The original signature of the provider requesting/performing/dispensing this service/item must appear in this element.
Element 27 — Date Signed
Enter the month, day, and year the PA/RF was signed (in MM/DD/CCYY format).
 Topic #4619 Prior Authorization Request Form Completion Instructions for Pharmacy Services and Diabetic Supplies
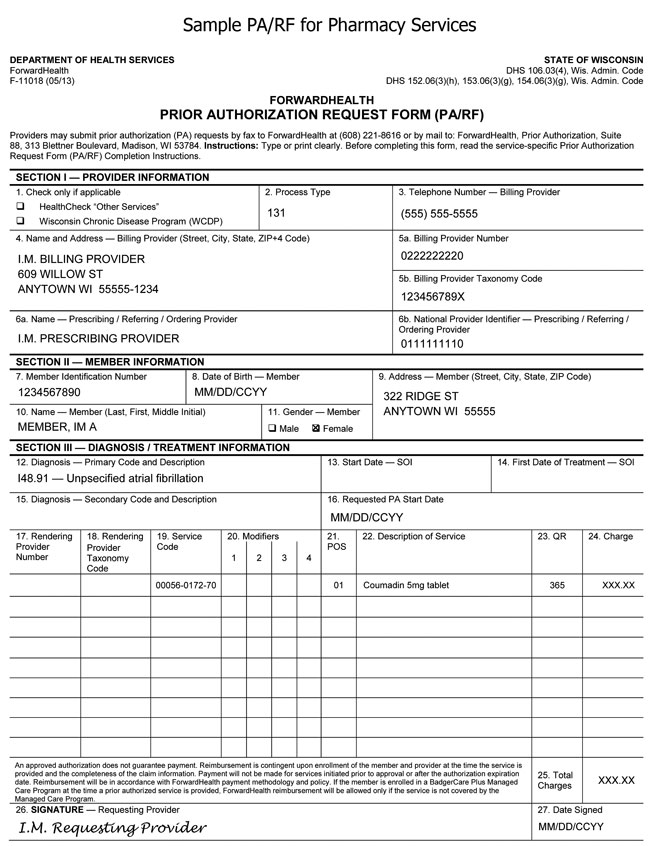
A sample PA/RF for pharmacy services is available.
ForwardHealth requires certain information to enable the programs to authorize and pay for medical services provided to eligible members.
Members of ForwardHealth are required to give providers full, correct, and truthful information for the submission of correct and complete claims for reimbursement. This information should include, but is not limited to, information concerning enrollment status, accurate name, address, and member
identification number (Wis. Admin. Code § DHS 104.02[4]).
Under Wis. Stat. § 49.45(4), personally identifiable information about program applicants and members is confidential and is used for purposes directly related to ForwardHealth administration such as determining eligibility of the applicant, processing PA requests, or processing provider claims for reimbursement. The use of the PA/RF is mandatory to receive PA for certain items. Failure to supply the information requested by the form may result in denial of PA or payment for the service.
Providers should make duplicate copies of all paper documents mailed to ForwardHealth. Providers may submit PA requests, along with all applicable service-specific attachments, via the ForwardHealth Portal, by fax to ForwardHealth at 608-221-8616, or by mail to the following address:
ForwardHealth
Prior Authorization
Ste 88
313 Blettner Blvd
Madison WI 53784
The provision of services that are greater than or significantly different
from those authorized may result in nonpayment of the billing claim(s).
SECTION I ― PROVIDER INFORMATION
Element 1 — HealthCheck "Other Services" and Wisconsin Chronic Disease
Program (WCDP)
Enter an "X" in the box next to HealthCheck "Other Services" if the
services requested on the PA/RF are for HealthCheck "Other Services." Enter an "X" in the box next to
WCDP if the services requested on the PA/RF
are for a WCDP member.
Element 2 — Process Type
Enter the process type 131 — Drugs. The process type is a three-digit code
used to identify a category of service requested.
Element 3 — Telephone Number — Billing Provider
Enter the telephone number, including the area code, of the office, clinic,
facility, or place of business of the billing provider.
Element 4 — Name and Address — Billing Provider
Enter the name and complete address (street, city, state, and ZIP+4 code)
of the billing provider. Providers are required to include both the ZIP code
and the four-digit extension for timely and accurate billing. The name listed
in this element must correspond with the billing provider number listed in
Element 5a.
Element 5a — Billing Provider Number
Enter the NPI of the billing provider. The
NPI in this element must correspond with the provider name listed in Element
4.
Element 5b — Billing Provider Taxonomy Code
Enter the national 10-digit alphanumeric taxonomy code that corresponds to
the NPI of the billing provider in Element 5a.
Element 6a — Name — Prescribing / Referring / Ordering Provider
Enter the prescribing provider's name.
Element 6b — National Provider Identifier — Prescribing / Referring / Ordering Provider
Enter the prescribing provider's 10-digit NPI.
SECTION II ― MEMBER INFORMATION
Element 7 — Member Identification Number
Enter the member ID. Do not enter any other numbers or letters. Use the
ForwardHealth identification card or Wisconsin's EVS to obtain the correct number.
Element 8 — Date of Birth — Member
Enter the member's date of birth in MM/DD/CCYY format.
Element 9 — Address — Member
Enter the complete address of the member's place of residence, including
the street, city, state, and ZIP code. If the member is a resident of a
nursing home or other facility, include the name of the nursing home or
facility.
Element 10 — Name — Member
Enter the member's last name, followed by their first name and middle
initial. Use the EVS to obtain the correct spelling of the member's name. If
the name or spelling of the name on the ForwardHealth card and the EVS do not
match, use the spelling from the EVS.
Element 11 — Gender — Member
Enter an "X" in the appropriate box to specify male or female.
SECTION III — DIAGNOSIS / TREATMENT INFORMATION
Element 12 — Diagnosis — Primary Code and Description
Enter the appropriate ICD diagnosis code and description with the highest level of specificity most relevant to the service/procedure requested. The ICD diagnosis code must correspond with the ICD description.
Element 13 — Start Date — SOI (not required)
Element 14 — First Date of Treatment — SOI (not required)
Element 15 — Diagnosis — Secondary Code and Description
Enter the appropriate secondary ICD diagnosis code and description with the highest level of specificity most
relevant to the service/procedure requested, if applicable. The ICD diagnosis code must correspond with the ICD description.
Element 16 — Requested PA Start Date
Enter the requested start DOS in MM/DD/CCYY format, if a specific start date is requested.
Element 17 — Rendering Provider Number
Enter the provider ID of the provider who will be performing the service,
only if this number is different from the billing provider ID listed in
Element 5a.
Element 18 — Rendering Provider Taxonomy Code
Enter the national 10-digit alphanumeric taxonomy code that corresponds to
the provider who will be performing the service, only if this code is
different from the taxonomy code listed for the billing provider in Element
5b.
Element 19 — Service Code
Enter the appropriate NDC for each
service/procedure/item requested.
Element 20 — Modifiers
Enter the modifier(s) corresponding to the service code listed if a modifier
is required.
Element 21 — POS
Enter the appropriate place of service code designating where the requested item would be
provided/performed/dispensed.
Element 22 — Description of Service
Enter a written description corresponding to the appropriate NDC for
each item requested.
Element 23 — QR
Enter the appropriate quantity (for example, days' supply) requested for the
procedure code listed.
Element 24 — Charge
Enter the provider's usual and customary charge for each
service/procedure/item requested. If the quantity is greater than "1.0,"
multiply the quantity by the charge for each service/procedure/item requested.
Enter that total amount in this element.
Note: The charges indicated on the request form should reflect
the provider's usual and customary charge for the procedure requested.
Providers are reimbursed for authorized services according to provider
Terms of Reimbursement issued by the Wisconsin DHS.
Element 25 — Total Charges
Enter the anticipated total charges for this request.
Element 26 — Signature — Requesting Provider
The original signature of the provider requesting/performing/dispensing
this service/procedure/item must appear in this element.
Element 27 — Date Signed
Enter the month, day, and year the PA/RF was signed (in MM/DD/CCYY format).
 Topic #449 Supporting Clinical Documentation
Certain PA requests may require additional supporting clinical documentation to justify the medical necessity for a service(s). Supporting documentation may include, but is not limited to, X-rays, photographs, a physician's prescription, clinical reports, and other materials related to the member's condition.
All supporting documentation submitted with a PA request must be clearly labeled and identified with the member's name and member identification number. Securely packaged X-rays and dental models will be returned to providers.
Photographs submitted to ForwardHealth as additional supporting clinical documentation for PA requests will not be returned to providers and will be disposed of securely. |